Detecting cancer
How Oxford's experts are changing the way we discover and diagnose different cancers
Cancer is easier to treat if it’s diagnosed early.
With late diagnosis resulting in a higher risk of death, detecting disease and starting treatment as early as possible is crucial to improve patient outcomes.
Almost half of all cancer cases in England in 2018 were diagnosed at stage III and IV. For some cancers this dramatically reduces the patient’s change of survival.
Researchers at the University of Oxford are using big data and artificial intelligence to improve our understanding of cancer-causing factors and implement risk tools for use in clinical settings by GPs.
They’re also developing tests that can diagnose multiple cancers at once in a simple, non-invasive way. The speed, availability and wide-ranging diagnostic abilities of these tests could help improve rates of early diagnosis, ultimately saving numerous lives.
Experts are investigating the patterns of non-specific symptoms and the chances of developing disease, as well as helping drive up early detection rates for childhood, teen and young adult (TYA) cancers.
Early cancer detection


A key strategic theme for Oxford Cancer, the University’s cancer research network, early detection is one of the areas benefitting from an £11 million award for the CRUK Oxford Centre.
Early detection seeks to identify those at highest risk of developing cancer and assess the best possible course of action for them. A number of approaches can be used to detect cancer earlier, including population-wide screening programmes, surveillance of people with high-risk conditions, and education about the warning signs of potential cancer.
Through the Oxford Centre for Early Cancer Detection, a multidisciplinary community of researchers and clinicians are working together to address NHS England’s long-term plan to detect 75% of cancers at an early stage by 2028.
The Centre’s research aims to help identify cancer earlier, allowing patients to benefit from treatment that is likely to cure them with fewer adverse side effects, and reduce the economic burden that advanced cancer brings.
Detecting cancer by blood test
One Oxford project seeking to improve early detection is SYMPLIFY.
This clinical trial seeks to evaluate the multi-cancer blood test Galleri, which can detect DNA from cancerous cells and tumours (ctDNA) at early stages.
The study, which recruited participants from 13 NHS trusts in England and 19 district hospitals in Wales, will test whether Galleri, which can detect over 50 types of cancer, could be used in GP visits.
‘Ultimately these tests could transform cancer patient care within the next five years by improving the chance of successful treatment and survival’
If the results from this and other trials are positive, Galleri could potentially improve the chance of successful treatment and decrease the need for invasive biopsies and expensive imaging.
Using epigenetics to detect cancer sooner
Diagnostic tests like Galleri are less invasive than current methods and would allow cancer testing to be performed more frequently on more people. The challenge, however, is sensitivity and specificity.
To ensure reliability, investigative procedures need to be able to detect the very low levels of ctDNA in blood and differentiate it from normal DNA. One approach is to sequence the circulating DNA; another is to look for cancer-specific patterns of epigenetic changes.
Epigenetics:
The study of heritable changes that are not the result of changes in the DNA sequence
The clinical application of epigenetic profiling has so far been limited by existing techniques’ dependency on bisulphite, a harsh chemical that degrades DNA samples, lowering sensitivity.
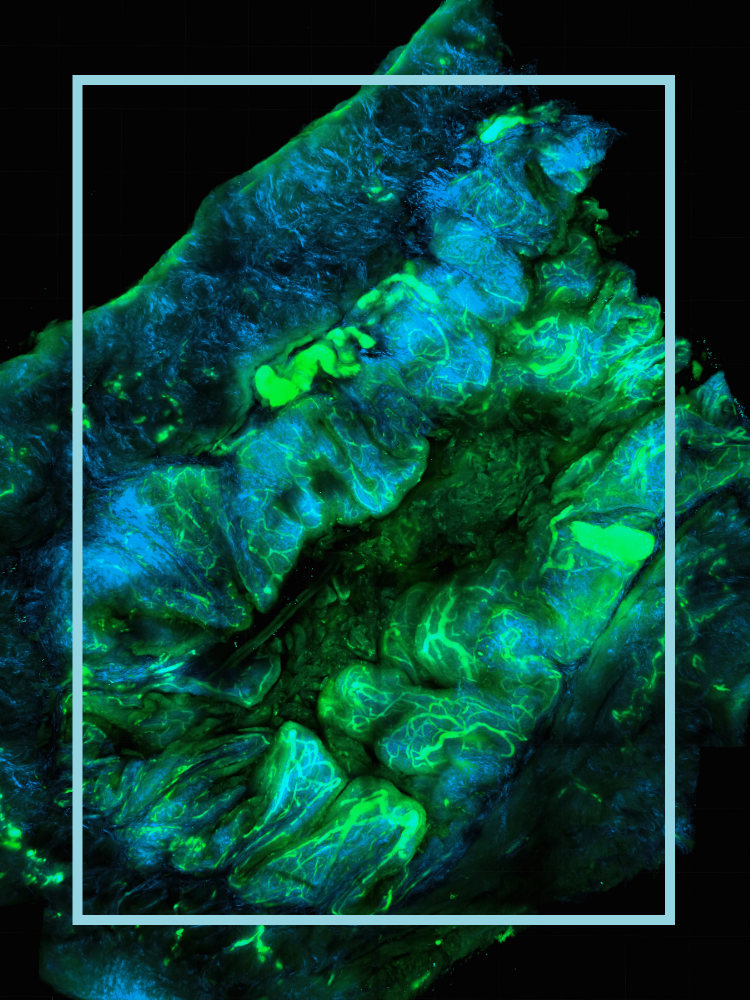
To resolve these issues, a bisulphite-free sequencing method called TAPS has been developed by Dr Chunxiao Song and Dr Benjamin Schuster-Böckler.
Thanks to support from the NIHR Oxford Biomedical Research Centre, Ludwig Cancer Research (Oxford Branch) at the Nuffield Department of Medicine, Dr Song’s CRUK-OHSU Award and the DeLIVER programme, TAPS is being tested on a variety of cancers, including liver, pancreatic and oesophageal.
Funding has also been provided to Dr Benjamin Schuster-Böckler and Visiting Fellow Professor Gerton Lunter to develop algorithms that can simultaneously detect genetic mutations and epigenetic changes from TAPS data.
This would increase the possibility of using combined genetic and epigenetic data to aid earlier cancer detection.
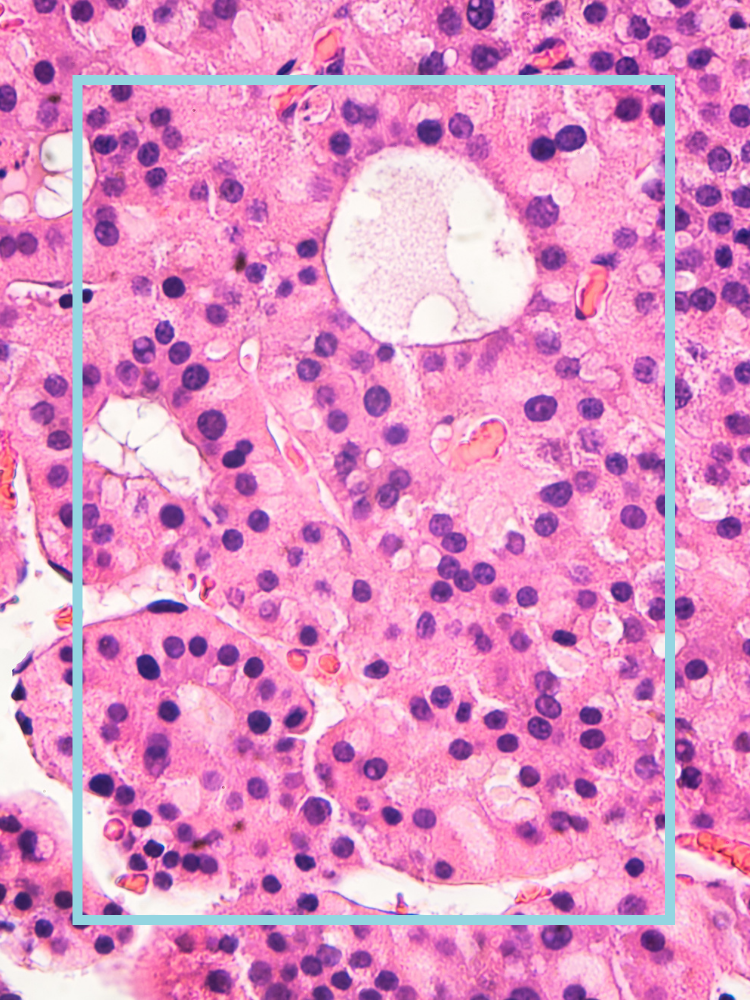
Identifying early indications of liver cancer
Hepatocellular carcinoma (HCC), cancer that begins in the liver, is one of the fastest rising causes of cancer death worldwide, with 854,000 new cases and 810,000 deaths per year. Its relatively low survival rate means earlier detection strategies are required urgently.
The DeLIVER programme, funded by a five-year Cancer Research UK Early Detection and Diagnosis Programme Award, aims to better understand the changes within the liver that lead to cancer, and to detect liver cancer at the earliest stage possible.
Led by Professor Eleanor Barnes of the Nuffield Department of Medicine, DeLIVER will use a variety of techniques to identify the earliest indications of HCC:
- Samples will be taken from the livers of people with and without cancer to compare how their liver cells are functioning in great detail as part of the Deep Liver Phenotyping and Immunology (DELPHI) study.
- The detection of Small Early Liver cancer with Natural history follow up (SELiNa) study will use new imaging technologies to identify those most at risk and detect small tumours.
- The Prospective Cohort for Early Detection of Liver Cancer (PEARL) study will assess whether the technologies identified in the SELiNa trial are able to detect liver cancers at early stages, and develop new prediction models that can identify patients most at risk.
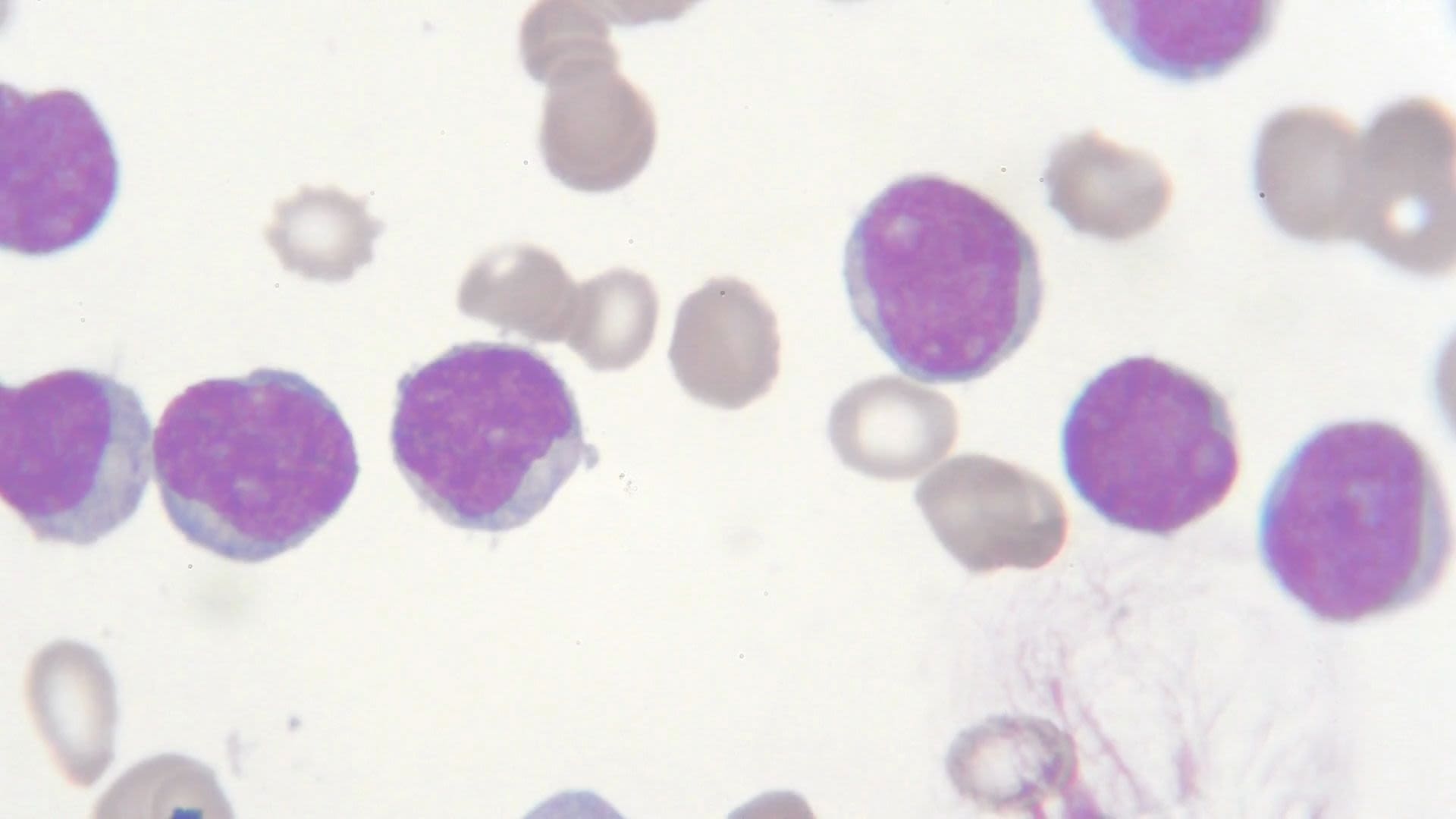
Lymphoproliferative disorders are another avenue for Oxford Cancer’s experts to investigate how to detect different types of cancer earlier.
Lymphoproliferative disorders:
Conditions in which the immune system may produce abnormal lymphocytes (a type of white blood cell) or proteins in the blood
Most lymphoproliferative abnormalities do not turn into serious conditions: only 1–2% of people may go on to develop blood or bone marrow cancer. However, there is no reliable way to predict who they are.
The Oxford Pre-Cancerous Lymphoproliferative Disorders (OxPLoreD) study is aiming to learn more about people with early-stage lymphoproliferative disorders and the factors that might predict cancer progression.
Detecting changes in disease and investigating non-specific symptoms
One of the reasons that ovarian cancer has a five-year survival rate of less than 50% is that many women (two thirds in the UK) are first diagnosed at an advanced stage.
A study by researchers from Oxford Population Health’s Cancer Epidemiology Unit has highlighted the importance of early diagnosis for ovarian cancer, and also looked at whether other factors – such as age, lifestyle factors and the microscopic structure of the cancer – affect survival.
‘The results indicate that tackling obesity and smoking could be one strategy to improve survival; however, the strongest association with stage suggests that earlier diagnosis would have a greater impact’
Using data from the Million Women Study, the researchers found that more advanced tumours were strongly associated with worse survival. Women diagnosed at stage IV had ten times the risk of death overall compared to women diagnosed at stage I. For women at stage III, the risk was seven times higher.
A study led by Nina Wietek, a CRUK Clinical Research Fellow and final year DPhil student from the Ahmed Lab, is seeking to understand the progression of mutation in ovarian cancer in order to detect it earlier by examining fallopian tube tissue.
Weight loss as a symptom of cancer
One of the issues with detecting cancers early is the presentation of non-specific symptoms such as bloating, abdominal pain, weight loss and weight gain.
‘Streamlined services that allow GPs to investigate non-specific symptoms like weight loss are vitally important and urgently needed if we are to catch cancer earlier and save lives’
Funded by the National Institute for Health and Care Research (NIHR), a study by the Universities of Oxford and Exeter found that weight loss was linked to ten types of cancer, and was the second highest risk factor for colorectal, lung, pancreatic and renal cancers.
Further studies confirmed the importance of weight loss as a symptom of cancer, regardless of the interval over which it occurs. Weight loss was associated with five types of cancer (pancreatic, myeloma, gastro-oesophageal, colorectal and breast), and with cancers at stage III and IV.
Could the onset of diabetes mean a future diagnosis of cancer?
The onset of diabetes is another possible indication of pancreatic cancer. More than a quarter of patients who develop pancreatic cancer will have had a diagnosis of diabetes in recent years or months.
Currently, more than half of people with pancreatic cancer die within three months of diagnosis.
Oxford research, funded by Pancreatic Cancer UK, is investigating whether those who have newly been diagnosed with diabetes are more likely to have, or go on to develop, pancreatic cancer.
The team will use information from the QResearch database, which contains the anonymised GP records of 35 million patients in England. This will be linked to hospital records, and cancer and death registries to locate individuals with ‘new-onset’ diabetes who have gone on to be diagnosed with pancreatic cancer.
Finally, they will compare the accuracy of their risk prediction using algorithms to establish whether a risk-based tool for GPs could be effective at detecting earlier stage pancreatic cancers in new-onset diabetes patients.
Detecting myeloma
Another of the cancers where weight loss could be a potential early indicator is a blood cancer, myeloma. However, weight loss is just one of a number of non-specific symptoms – including back pain and tiredness – that could be presenting due to cancer.
These symptoms aren’t limited to myeloma, meaning patients might visit their GP on more than one occasion to rule out other more common causes. Associate Professor of Haematology Dr Karthik Ramasamy, along with colleagues from Amgen Ltd and Aetion, studied electronic records of more than 2,500 patients with the aim to accelerate myeloma diagnosis.
Haematology:
The study of blood and blood-forming tissues and the disorders associated with them
This work identified common early clinical features of subsequent myeloma diagnoses, and can be used to increase awareness of the need for earlier recognition and testing of myeloma in primary care.
Previous studies into myeloma indicated that myeloma could be detected earlier using blood tests. Funded by the NIHR, a study conducted by the Universities of Oxford and Exeter demonstrated that a combination of two blood parameters could be sufficient for diagnosis, with such blood tests being routinely conducted by GPs.
The study’s lead author, Dr Constantinos Koshiaris, says that, if abnormalities are detected in the tests, patients should receive urgent urine protein tests, which could help speed up diagnosis.
Making testing for cancer less invasive
Dr Jennifer Allen and Karen Billington from the Goberdhan Lab are investigating whether they can use extracellular vesicles (EVs) to detect oesophageal cancer, and whether EV information could be extracted and tested through simple blood tests.
Vesicle:
A small, usually fluid-filled, membrane-bound sac within the cytoplasm of a living cell
Patients with Barrett’s Oesophagus, a pre-cancerous condition in which oesophageal cells become damaged, require monitoring to allow the early detection of oesophageal cancer. Currently, the monitoring process involves invasive and costly endoscopy.
Working with Dr Elizabeth Bird-Lieberman at Oxford’s John Radcliffe Hospital, the team are collecting samples from patients with Barrett’s Oesophagus, to see if EV information can be extracted and tested through blood tests.



Diagnosing different cancers
One test, multiple cancers
Early detection is a crucial step in improving patient outcomes, but with more than 200 known types of cancer, some presenting with non-specific symptoms, it can be difficult to know what to test for.
Professor Jason Davis, working alongside clinicians, is focusing on developing a handheld diagnostic test that has the potential to test for many types of cancer all at once – at an earlier, pre-symptomatic stage.
The test uses electroanalytical methods to detect biomarkers. A single drop of blood can be analysed directly, and results are generated within a few minutes.
Biomarker:
A naturally occurring molecule, gene or characteristic by which a particular pathological or physiological process, disease, etc. can be identified
The spinout company Osler Diagnostics came from the work of Professor Davis’s lab, and aims to develop this technology into a clinically implementable system for GP surgeries to use in testing for disease in asymptomatic individuals.
Accelerating the diagnosis of people with non-specific cancer symptoms is also the focus of the Suspected CANcer (SCAN) pathway, based at the Churchill Hospital.
Led by Dr Brian Nicholson and Professor Fergus Gleeson, SCAN performs CT scans, and blood and stool tests, on patients referred by their GP.
As well as having diagnosed over 300 incidences of cancer, the SCAN pathway directly informed the specification of the NHS’s new Rapid Diagnostic Centres and the Welsh Single Cancer Pathway. The SCAN team won the British Medical Journal Awards 2020 Cancer Care Team of the Year as a result.
SCAN was also the first and only non-specific symptoms pathway to develop a research database including comprehensive imaging, lab and clinical data, and biobanking of blood and urine samples. SCAN’s research infrastructure underpins several projects at Oxford, including the SYMPLIFY clinical trial.
It also underpinned the work that went into developing the first ever blood-based test to simultaneously identify if a patient has cancer, and if that cancer has spread.
‘This work describes a new way of identifying cancer. The goal is to produce a test for cancer that any GP can request.’
The test, which analysed 300 patients recruited through the SCAN pathway, can be used to detect a range of cancers, and whether they have metastasised (spread). It is the first technology to be able to determine the metastatic status of a cancer from a blood test, without already knowing the primary cancer type.
It shows promise in helping clinicians detect cancer and assess cancer stage in the future. Rapid and inexpensive, it could help overcome many barriers to the early detection of cancer, especially in patients with non-specific symptoms.
Specific tests for specific cancers
Whether specific to one cancer, or non-specific to many, it’s important to understand which symptoms could indicate a risk of disease in order to increase the likelihood of early diagnosis.
For example, research by Professor Julia Hippisley-Cox and Dr Weiqi Liao highlighted 21 signs of pancreatic cancer, two of which were previously unrecognised – feeling thirsty and having dark urine. The findings can also be used to update QCancer, a tool created from the QResearch database that helps GPs identify high-risk patients.
A team of researchers led by Professor Hippisley-Cox and Dr Shivan Sivakumar also studied how pancreatic ductal adenocarcinoma (PDAC) risk factors vary over time leading up to diagnosis.
Using the QResearch database, the team looked at 28,137 people before their PDAC diagnosis, comparing their body mass index, blood-based markers, other illnesses and medication use with 261,219 matched controls.
Another study, led by Dr Christiana Kartsonaki, used data from the China Kadoorie Biobank, which includes over 500,000 Chinese adults, to identify protein biomarkers for pancreatic cancer. The study found several proteins in blood that are associated with an increased risk of pancreatic cancer, which could be used to improve risk prediction models, especially in the short term.
‘Earlier detection, even if only by a few months, could benefit patients and may allow the use of treatments such as surgery’
Current prostate cancer detection relies on a prostate-specific antigen screening blood test. Although it has been proven to reduce deaths from the disease, it can also produce false-positive results, encouraging over-detection of slow-growing, non-aggressive tumours.
Using the QResearch database, Professor Julia Hippisley-Cox and Professor Carol Coupland (University of Nottingham) developed a tool to calculate personalised risk of prostate cancer.
Using the records of 1.45 million men, their new prediction algorithm aims to diagnose tumours at an earlier stage, when they’re easier to treat.
Genetic testing can also better inform when men should undergo screening for prostate cancer. Work co-authored by Dr Ian Mills, John Black Associate Professor of Prostate Cancer, aims to detect who should be screened at what age.
Using genome-wide association studies, genetic variations in the DNA 31,747 men were incorporated into a new prediction tool, the Polygenic Hazard Score. This can estimate genetic risk; as an individual’s genotype does not change with age, it can be used to decide whether, and when, a man should undergo screening for prostate cancer.
‘We can advance the adoption of powerful technology to help pathologists by demonstrating the system-wide potential of using AI-based diagnostic systems in routine reporting’
Researchers from Oxford University are also evaluating a prostate cancer detection software system that may be able to help pathologists quickly identify suspicious areas of tissue. The system, developed by Paige Prostate, allows doctors to quickly identify whether cancer is present in a biopsy by automatically detecting and highlighting areas of suspicious tissue.


Cancer big data
Through the interrogation of vast amounts of data about patients and their tumours, and the successful integration of data science, Oxford Cancer researchers are seeking to revolutionise the scale and efficiency of cancer research.
Over 60 research groups in Oxford are focusing on the application of data science to cancer research, spread across teams from the Big Data Institute to the Mathematical Institute. They specialise in diverse data types, including health records, molecular genetics and images.
Data is being collected and analysed on things as small as individual molecules, and as large as population-scale studies. They range from the Oxford-based Million Women Study and China Kadoorie Biobank, through to information from the National Consortium of Intelligent Medical Imaging (NCIMI), the NIHR Health Informatics Collaborative and NHS Digital.
Their work identifies factors that correlate with cancer diagnosis, treatment response and outcomes. It informs public health policy, treatment selection and screening programmes.
Experts are applying mathematical modelling and simulations, making the integration of computational biology routine in cancer research. They’re also ensuring that, as research and diagnostic technologies develop, cancer images are widely available for use in cutting-edge approaches, and these analyses are translated into clinical environments and future research.


Detection technology

The need to improve artificial intelligence
There is an increasing drive towards digital pathology in clinical settings. As a result, there has been a surge in research and development tools for AI to support pathologists in diagnostics.
AI algorithms require training in order to ‘learn’ to identify problems. They use large datasets of images accompanied by clinical outcome data to do this.
However, research by academics from the Oxford University Hospitals NHS Foundation Trust has found that images and data available for training AI to spot skin cancer do not include enough images of darker skin.
Highlighting an urgent need for improved diversity and quality in skin datasets, researchers, led by Dr David Wen, found 21 freely accessible sets of data on skin lesions around the world, containing more than 100,000 pictures. Of the 21 datasets, 14 included information on which country patients in the images came from, but only a small percentage of the images were accompanied by information about skin colour or ethnicity.
Where skin colour was stated (2,436 images), only ten were of brown skin, and just one was of dark brown or black skin. Of the images with ethnicity stated, none came from patients of African, Afro-Caribbean or South Asian background.
AI and pathology
Currently, image quality control is reliant on pathologists to conduct manual assessment. Due to the scale of datasets needed, this is unsustainable.
Pathologists Dr Lisa Browning and Professor Claire Verrill, and biomedical engineers Dr Maryam Haghighat and Professor Jens Rittscher, teamed up to address this.
The Oxford-developed AI tool PathProfiler has been able to automate the quality control of large retrospective pathology image datasets, increasing their usability in research later on.
‘By using this AI tool to triage prostate biopsies for IHC, pathologists would spend less time reviewing these cases, which would not only lead to financial savings but it would also accelerate prostate cancer diagnosis to inform patients and treating clinicians earlier’
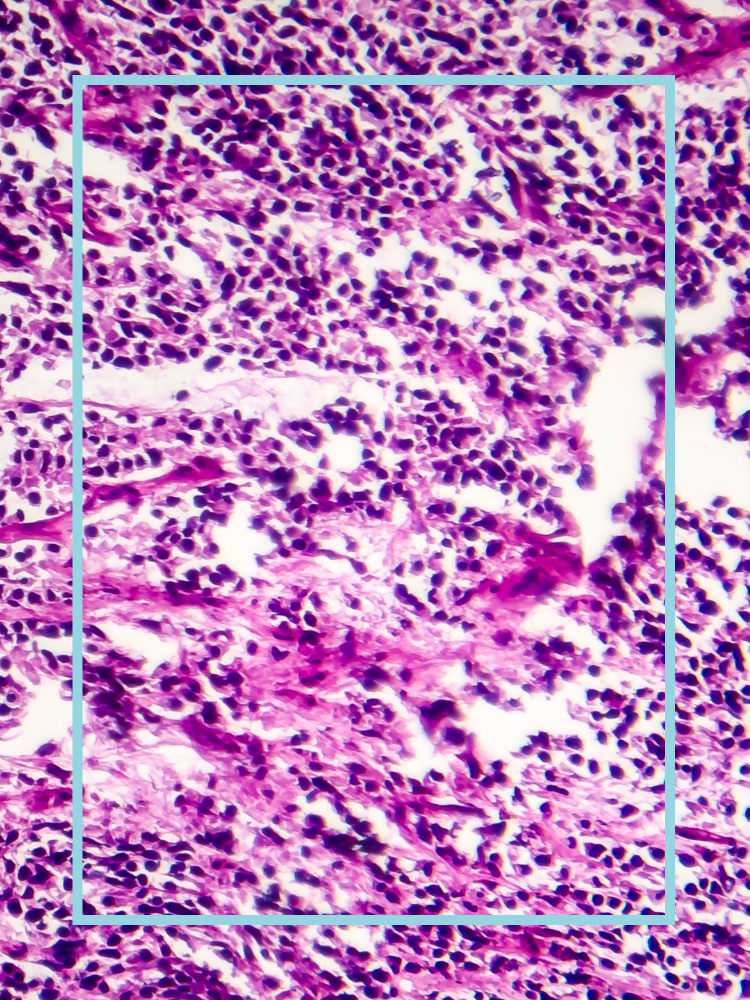
Previous related work by Professors Verrill and Rittscher, and Dr Lisa Browning, as well as colleagues Dr Richard Colling and Andrea Chatrian, used prostate biopsies annotated by Oxford University Hospital pathologists to train an AI tool to detect tissue regions with ambiguous morphology and decide which cases needed immunohistochemistry (IHC). IHC is the additional process of studying other cellular features, something that pathologists otherwise need to determine the need for, causing potential bottlenecks in pathology workflows.
Use of the tool, according to the researchers, would save 11 minutes of pathologist time for each case, which scales up to 165 hours per 1,000 prostate biopsies.
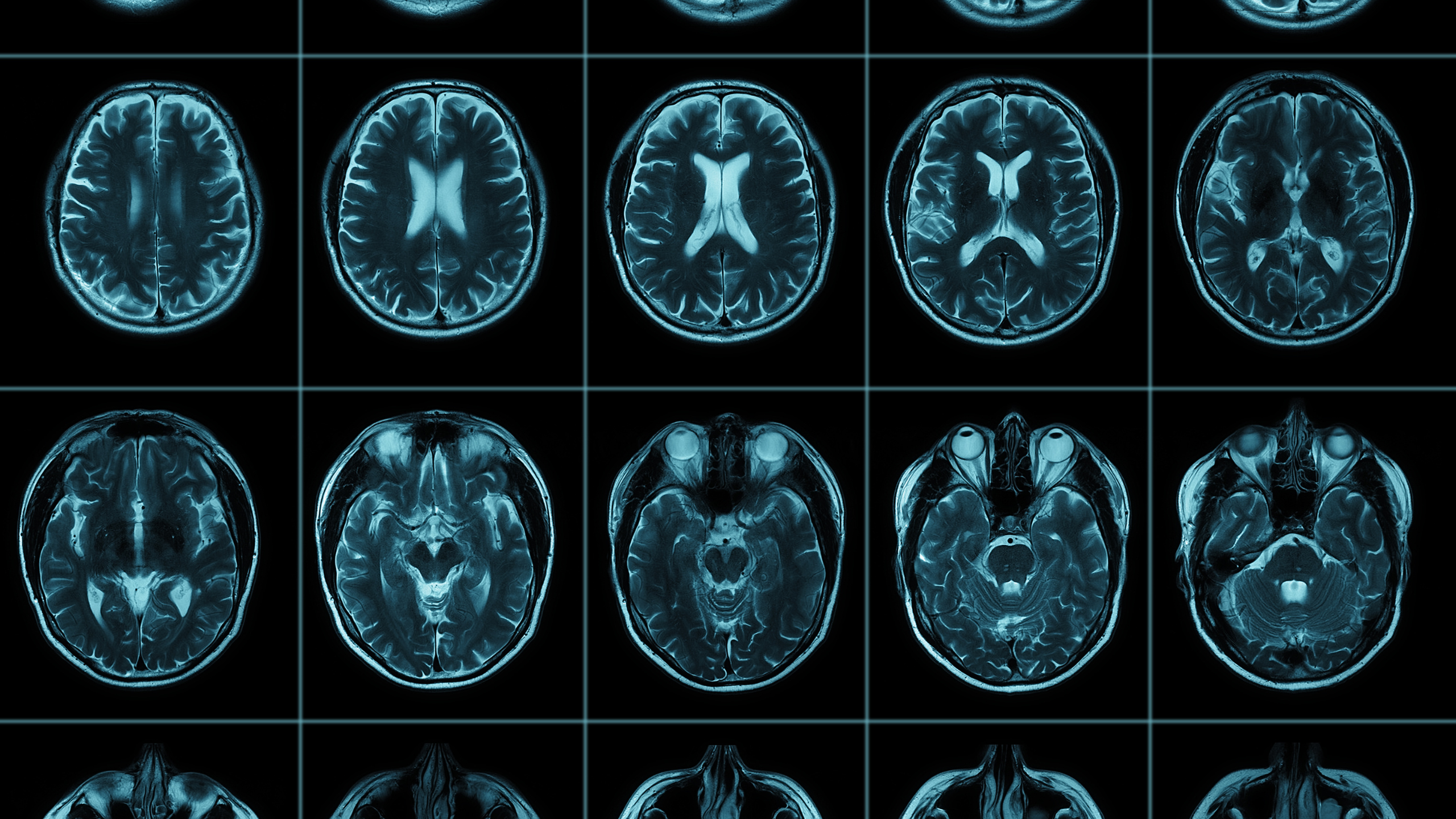
Detecting lung cancer earlier using artificial intelligence
Lung cancer is the biggest cause of cancer mortality in the UK. Only 19% of people live for one year after a stage IV diagnosis; this rises to 88% if the disease is caught at stage I.
Two research programmes led by the University of Oxford are focusing on improving the early diagnosis of lung cancer, thanks to funding from partners such as UK Research and Innovation, the NIHR, Cancer Research UK and industry partners.
The IDEAL project, led at Oxford by Professor Fergus Gleeson, is working in collaboration with colleagues from the Universities of Leeds, Nottingham and Reading, and the Oxford spin-out Optellum. The team are using AI to extract information about lung nodules from CT scans, and predicting whether they contain malignant cancer cells by comparing them to thousands of nodules with known diagnoses.
The DART project, again led by Professor Gleeson, is integrating clinical, imaging and molecular data using AI algorithms, with the aim of diagnosing lung cancer earlier and with more accuracy. The project also aims to improve patient selection for lung cancer screening and enable better assessment of risk from co-morbidities.
Both IDEAL and DART aim to support clinicians, improve outcomes for patients and save money for the NHS.
Along with colleagues from the University of Nottingham, Imperial College and a number of NHS trusts, researchers from the DART project are working with the Roy Castle Lung Cancer Foundation, and three industry partners – Roche Diagnostics, GE Healthcare, and again, Optellum.
Medtech company Optellum, co-founded by Professor Sir Michael Brady, achieved a CE certification under the EU’s Medical Device Regulation for its Virtual Nodule Clinic in early 2022.
Quantifying pre-cancerous risks through AI visualisation
AI can also help improve the results of tests that would otherwise be dependent on the skill and expertise of the individual carrying out the procedure.
Funded by the NIHR Oxford Biomedical Research Centre (BRC), researchers have been using AI alongside endoscopy to get more accurate readings of patients with Barrett’s oesophagus.
‘Most endoscopists don’t encounter an early Barrett’s cancer that often. So, instead of teaching thousands of endoscopists, by applying deep learning techniques to endoscopic videos you can teach a programme’
The system reconstructs the surface of a Barrett’s area in 3D from the endoscopy video, allowing the clinician to quantify it precisely. This understanding of the size of the affected area can help them determine cancer risk and how often a patient should be surveyed.
Analysing existing detection methods
Developing new and innovative methods of detection is important, but so too is the analysis and comparison of existing ones.
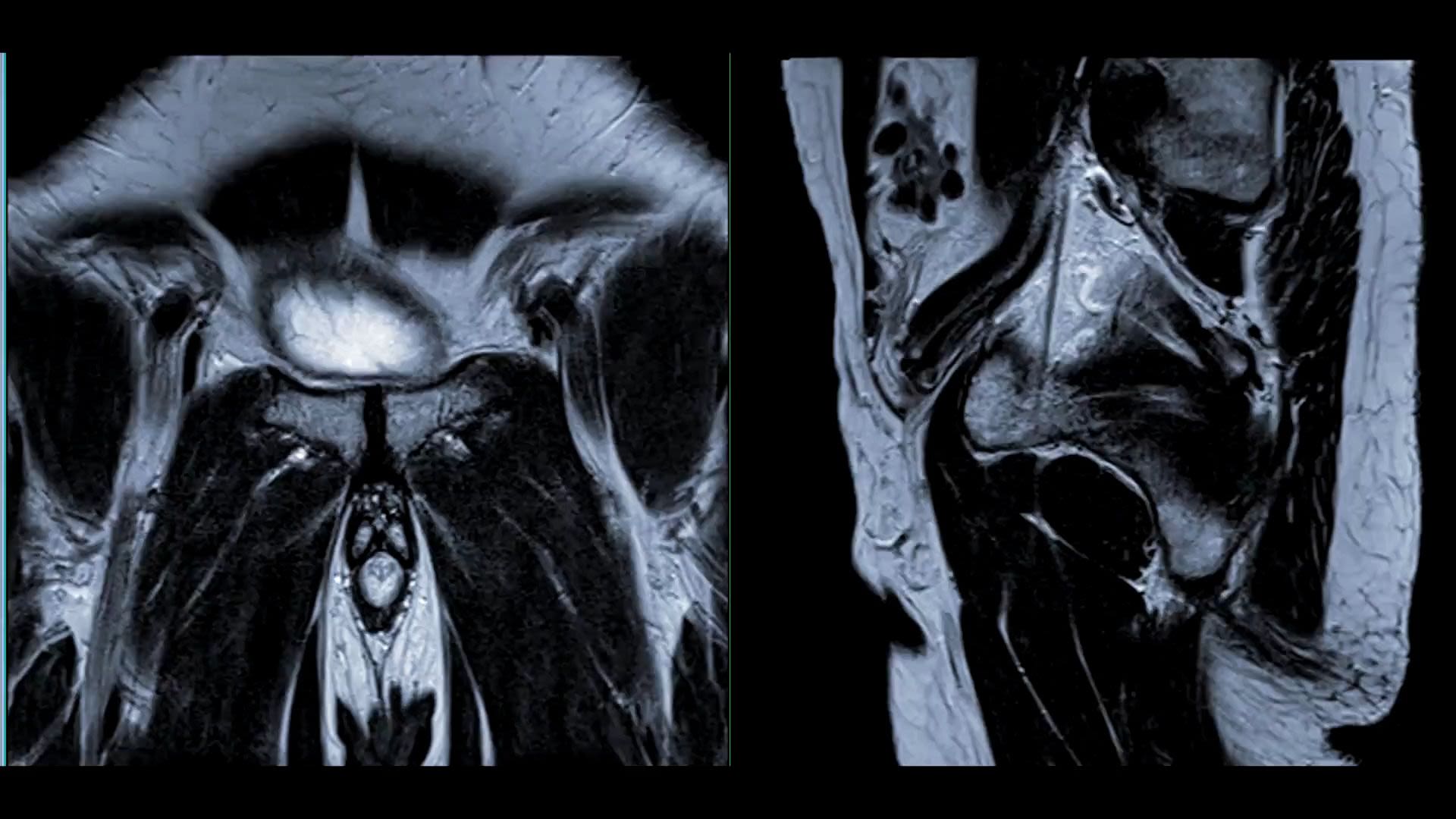
Research by the NIHR, and the Universities of Oxford, Bristol, Ottawa and Exeter, found that MRI scans to target biopsies are more effective at detecting prostate cancers that are likely to need to treatment than standard ultrasound-guided biopsies.
Combining results from seven studies of 2,582 patients, the researchers’ evidence supports the use of pre-biopsy MRIs for the diagnosis of suspected prostate cancer, something increasingly used in the UK, but not as commonly adopted globally.
Cancer in children and young adults

Using data to detect cancer in children and young adults
In the UK, the time in which it takes to diagnose childhood, teenage and young adult cancer lags behind other high-income countries; this delay worsens patient outcomes.
Funded by a Cancer Research UK Early Detection and Diagnosis Project Award, Dr Defne Saatci and Professor Julia Hippisley-Cox are exploring QResearch data to identify the early symptoms and signs associated with a subsequent diagnosis of most cancers in young people.
Detecting cancer in children and young adults in sub-Saharan Africa
Currently, 95% of global child lymphoma blood cancer cases are found in sub-Saharan Africa. A subset of these, called Epstein-Barr Virus-related (EBV) lymphomas, are particularly aggressive. This is the focus of AI-REAL, the global health program established by researchers at the University of Oxford.
Funded by the NIHR, the Aggressive Infection-Related East Africa Lymphoma (AI-REAL) project led by Professor Anna Schuh aims to bring the next generation of diagnostic technology to Tanzania and Uganda. They plan to improve the testing process for EBV lymphomas, subsequently increasing the chances of children’s early diagnosis and survival.
In partnership with four hospitals, new equipment has been installed and training programmes established. Live-streaming technology is used to share clinical knowledge with counterparts in Uganda and Tanzania.
‘The aim is not just to improve the diagnosis for these children, but also to build capacity so that DNA-based cancer diagnostics can be used across the board in sub-Saharan Africa’
The project, whose main research site is located in Northern Uganda, has created around 30 jobs for doctors, nurses, bioinformaticians and postgraduate students in health economics, biology and oncology.
In August 2022, the project conducted its first early diagnosis using liquid biopsy technology. A four-year-old from a remote area of Northern Uganda was diagnosed with Burkitt Lymphoma.
She was the very first patient recruited at Lacor, one of the four hospital sites, and is responding well to treatment.
Understanding how childhood cancer develops
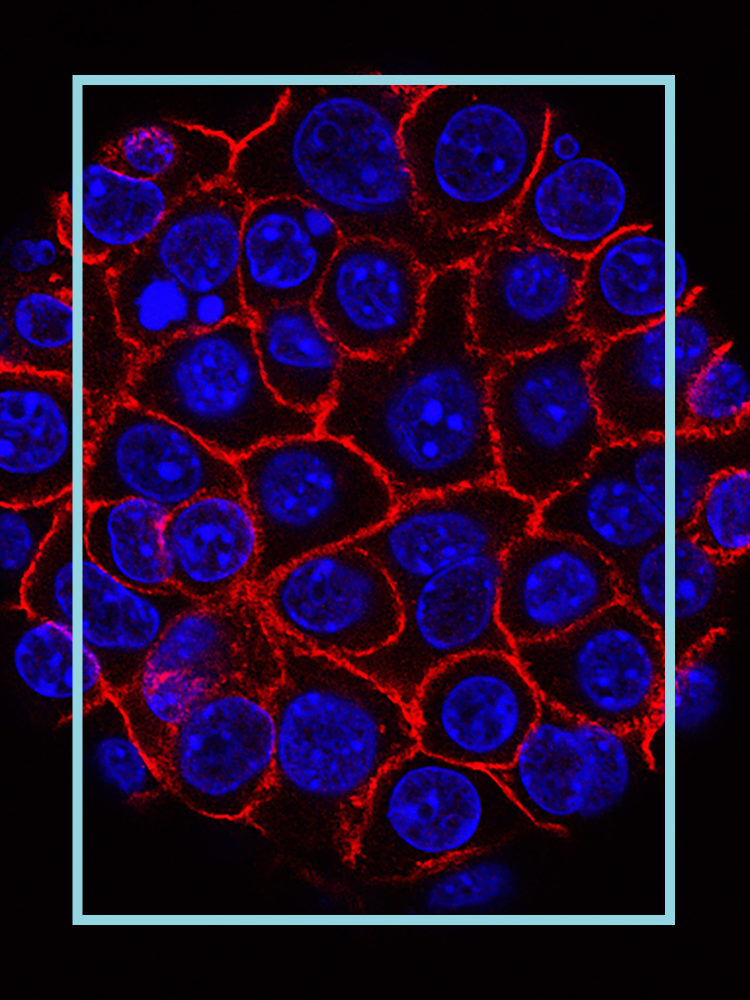
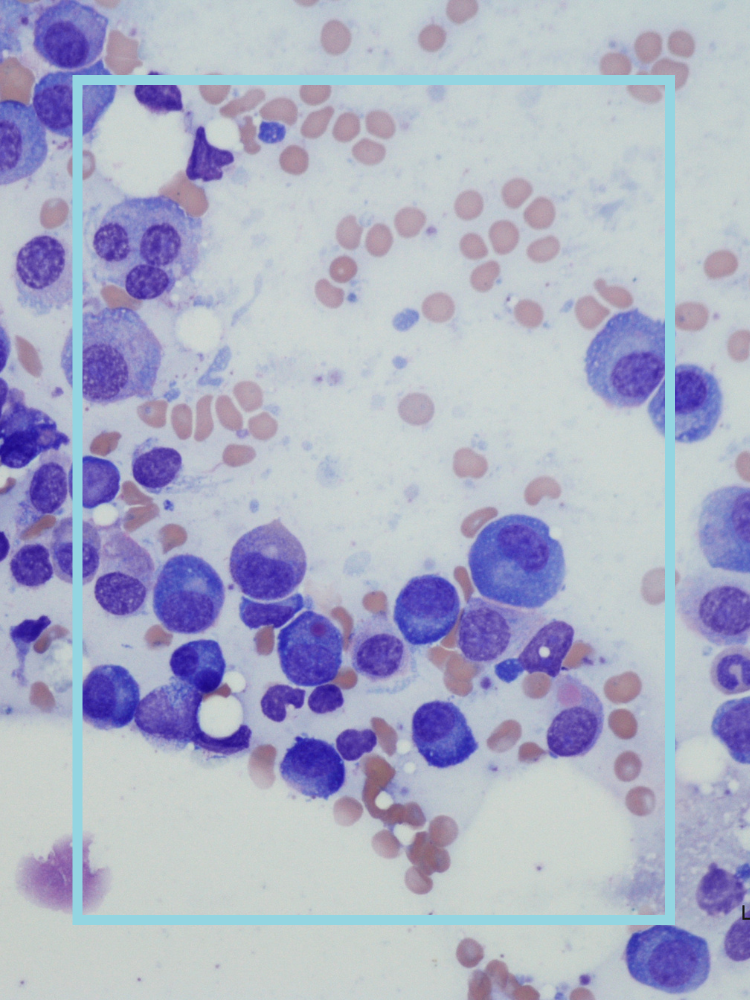
A method 20 years in the making could lead to the development of new treatments for infant Acute Lymphoblastic Leukaemia (ALL).
ALL is a cancer that affects white blood cells; it is one of the most common childhood cancers. Since the 1970s, mortality rates for ALL have decreased by almost half, and survival rates for children have risen to 90%. Unfortunately, for babies under one, ALL is more aggressive and less responsive to treatment – only 50–60% can be cured.
‘For the first time, we have a model where we can carefully map out the molecular details of this aggressive disease’
Professor Anindita Roy says that infant ALL has a unique biology, likely dependent on specific developmental features of the prenatal cells it arises in.
The breakthrough, made by researchers from the Roy, Roberts and Milne groups, focused on a genetic change found in around 70% of infant ALL cases, in which chromosomes become rearranged. The researchers were able to accurately replicate the clinical and molecular features of infant ALL, as well as shed light on why infant leukaemia is more aggressive.
Funded by the Medical Research Council (MRC), Blood Cancer UK, Wellcome and funding to individual authors, it’s hoped that the model will facilitate further insights into infant ALL, and be an essential preclinical tool that can manipulate vulnerabilities in infant ALL cells, and test novel therapies.
Work by Professor Irene Roberts, Professor Thomas Milne and Professor Anindita Roy is also supported by the NIHR Oxford Biomedical Research Centre.
‘We know this will ultimately help researchers develop better ways of treating, or even preventing, leukaemia in these children’
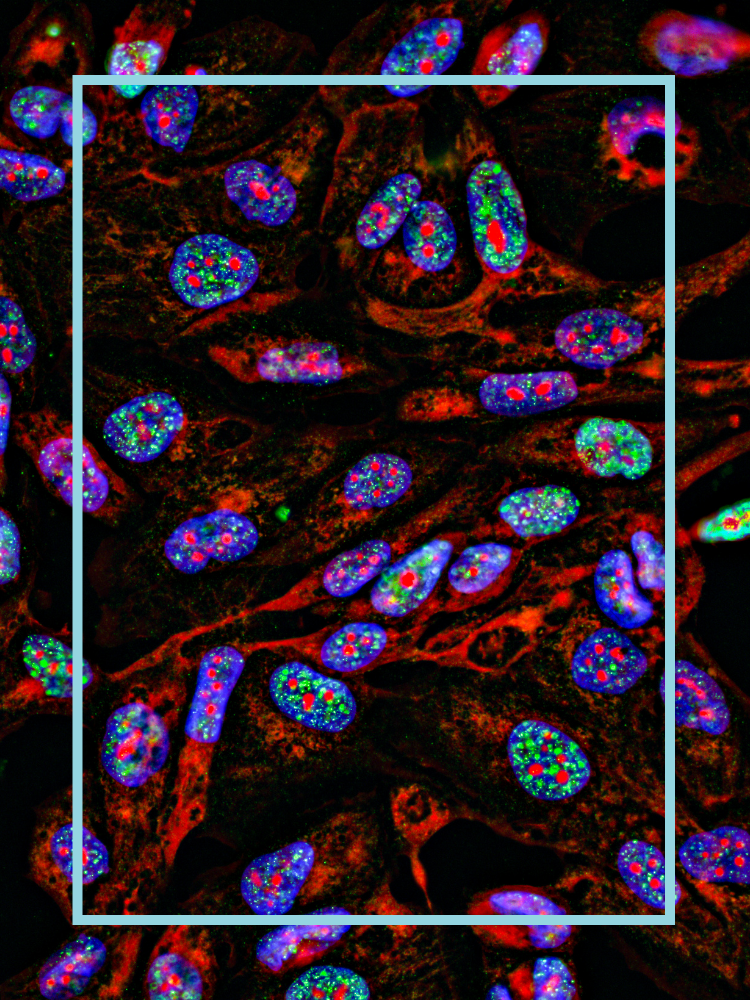
Professors Irene Roberts and Anindita Roy – both of the MRC Molecular Haematology Unit, the MRC Weatherall Institute of Molecular Medicine and the Department of Paediatrics – have also produced detailed analysis of the prenatal development of blood and immune cells in bone marrow.
Part of the Human Cell Atlas initiative to provide comprehensive reference maps of every human cell type, researchers from a number of institutions have pinpointed a 6–7 week window during the second trimester of pregnancy in which the full range of blood and immune cells are established in bone marrow.
For researchers exploring the blood and immune systems, this data will be a valuable reference, especially for those investigating the changes in the processes that lead to diseases such as cancer.
According to Professor Irene Roberts, the study characterises some of the differences in gene expression in the bone marrow, which will help researchers to figure out whether these differences are significant, and in what way.
For Professor Andi Roy, the project has also been important because of how the researchers have shown the utility of datasets in understanding the effects on human health of perturbed blood cell production processes.
This particular research was again funded by Wellcome and the MRC, with the work of Professor Irene Roberts and Professor Andi Roy being funded by the NIHR Oxford Biomedical Research Centre.