Disease and degeneration
Brain health is essential for physical and mental health, social wellbeing, productivity and creativity.
Diseases of the brain and nervous system can be impacted by genetic, environmental and lifestyle factors and are increasingly common and serious health problems of middle and old age.
Researchers at the University of Oxford are conducting world-leading research to uncover the underlying causes of such diseases, to slow disease progression and to develop transformative new treatments.
Disease and the brain
Oxford experts are investigating which parts of the brain are impacted by neurodegenerative diseases, in order to better understand their progression and potential treatments.
Neurodegenerative:
Resulting in or characterised by degeneration of the nervous system, especially the neurons in the brain
The cerebrum
Cerebral metabolism is fundamental for healthy neurological function.
In a collaborative study with researchers from the University of Cambridge and Aarhus University, Professor Damian Tyler, from the Department of Physiology, Anatomy and Genetics, and Dr Jack Miller, from the Radcliffe Department of Medicine, examined a novel approach to investigating alterations in the cerebral metabolism which may be a precursor and early biomarker of later stage neurological disease processes.
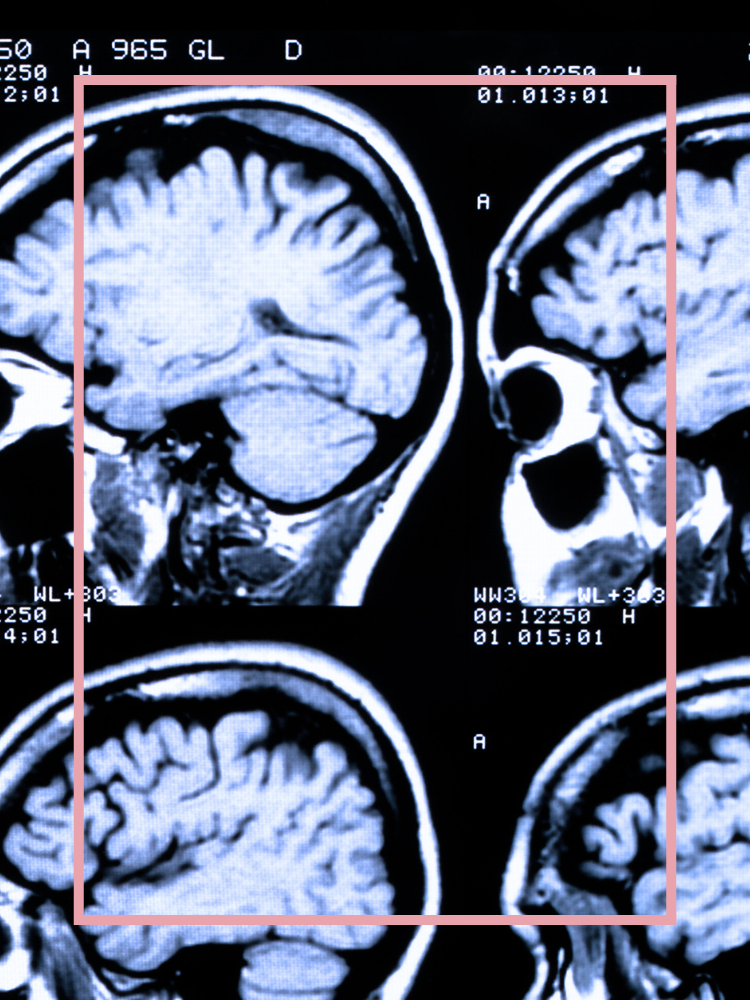
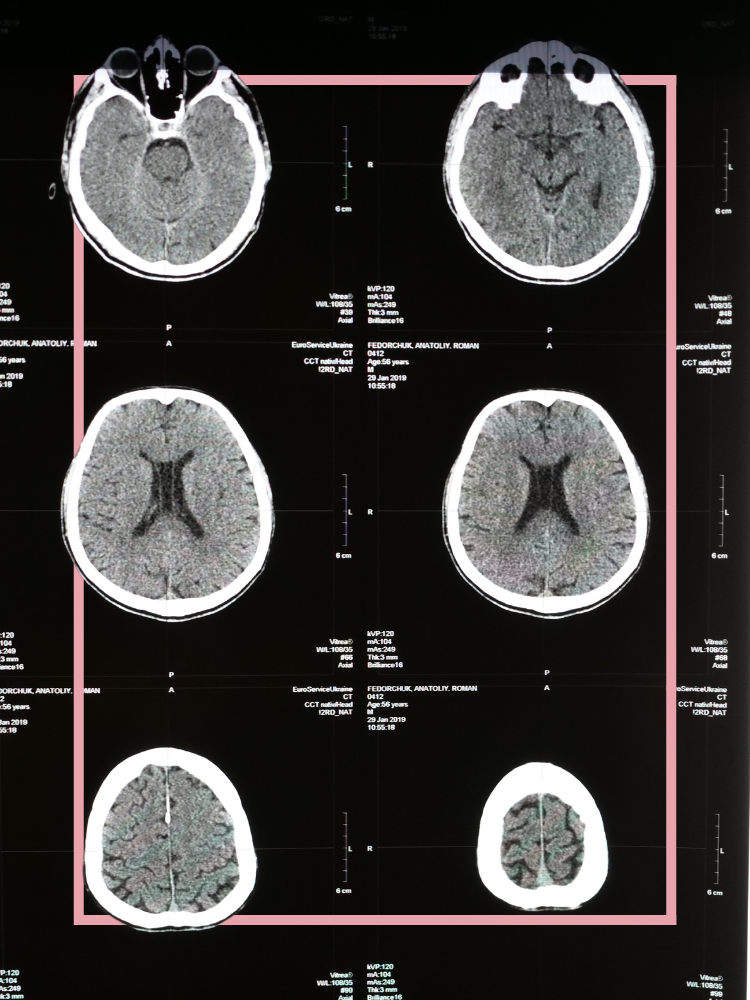
Hyperpolarized carbon-13 magnetic resonance imaging (CMRI) is an emerging clinical technique that could provide key insights into the viability of normal appearing tissues in the brain.
The cerebellum
The cerebellum is the primary centre of motor coordination and learning in the central nervous system.
The Cerebellar Disease Group, part of the Nuffield Department of Clinical Neurosciences, aims to understand the genetic, molecular and cellular mechanisms that underlie neurodevelopmental and neurodegenerative diseases of the cerebellum.
The group, led by Professor Esther Becker, is one of the few laboratories worldwide who have developed a robust protocol using stem cells to create 3D models of the cerebellum called organoids.
Dr Jussi Tolonen examines ataxia and other cerebellar movement disorders using cerebellar organoids.
Proteins
Neurodegenerative diseases such as Alzheimer’s or Parkinson’s are associated with the build-up of toxic proteins in the brain.
Emeritus Professor David Smith from the Department of Pharmacology co-founded the Oxford Project to Investigate Memory and Aging (OPTIMA).
In a paper written with Professor Helga Refsum the researchers examine how elevated levels of the amino acid homocysteine (tHcy) is associated with cognitive decline, white matter damage, brain atrophy, and increased risk of vascular dementia and Alzheimer's disease.
Their findings revealed that homocysteine may interact with both risk factors and protective factors, identifying people at risk but also providing potential strategies for early intervention.
Their findings gave scope for further research into whether simple interventions with nutrients can prevent progression to dementia.
The Kavli Institute for Nanoscience Discovery is Oxford’s first interdisciplinary science institute spanning the life, medical and physical sciences.
The Institute’s Brain Health research theme brings together scientists across disciplines to address major research challenges related to the brain, including improving understanding of the mechanisms underlying neurodegenerative conditions.
A recent collaborative study, led by Professor Richard Wade-Martins’ group in the Department of Physiology, Anatomy and Genetics, demonstrated for the first time that symptoms for Alzheimer’s can be predicted in preclinical models.
‘We are excited to have found that brain cells generated in the laboratory from individual Alzheimer’s patients reflect their clinical vulnerability to amyloid-beta. This will help us better understand mechanisms of resilience and will help in the search for new therapeutic strategies.’
The Molecular Neurodegeneration Research Group, part of the Nuffield Department of Clinical Neurosciences, was established by Professor George Tofaris with an aim to understand fundamental biological processes that could inform the development of targeted therapies and innovative biomarkers in neurodegenerative and neurogenetic disorders.
Neurogenetics:
The genetics of neural development or of neurological disorders; the branch of genetics dealing with the nervous system
One of the principal neuropathological features of Parkinson’s disease and dementia is the formation inside neurons of Lewy bodies.
These ‘bodies’ are clumps of a sticky protein called alpha-synuclein that build up in nerve cells in the brain, causing damage and eventually the death of these cells. Typically, they affect the brain cells that control movement. Professor Tofaris and his team have used a diverse set of investigations to model pathological process of proteins that leads to Parkinson’s disease.
‘Pharmacological inhibition of [the enzyme] Usp8 using small molecules could pave the way to novel therapeutics.’
Neurons
Neuroinflammatory conditions are all characterised by the gradual damage and loss of neurons, the cells that transmit signals from the brain and spinal cord to other parts of the body.
The Oxford Centre for Neuroinflammation, based in both the Nuffield Department of Clinical Neurosciences and Weatherall Institute for Molecular Medicine, is led by Professor Lars Fugger. The Centre brings together biomedical, analytical and clinical expertise to shed new light on the causes that underpin neurodegenerative diseases.
Researchers from the Centre, with colleagues from University of Hamburg, uncovered a disease-causing population of immune cells, which travel to the brain in patients with multiple sclerosis (MS).
‘Our results suggest that the colonisation of the brain by immune cells could be an important factor in the therapeutic resistance of late-stage MS…At the same time, we demonstrate that these cells can be mobilised to the blood at an early disease stage, raising the possibility that they could be reached by novel therapeutics.’
Blood-brain barrier
The blood-brain barrier is a protective layer between the brain’s blood capillaries and the cells that make up brain tissue. It’s thought that several neurological diseases could originate from a dysfunctional blood-brain barrier.
This barrier provides a defence against the pathogens and toxins that may be in our blood, allowing very few molecules to pass through; however it can also prevent many drugs from passing across into the brain, and this presents a major problem in treating neurological conditions.
A consortium of 27 partners, coordinated by the Nuffield Department of Clinical Neurosciences, is tackling the challenge of discovery and characterisation of blood-brain barrier targets and transport mechanisms for brain delivery of therapeutics to treat neurodegenerative diseases. IM2PACT is funded by the Innovative Medicines Initiative and is led in Oxford by Professor Zameel Cader.
‘…we will be able to develop more sophisticated models that replicate the human blood-brain barrier far more accurately, allowing us to investigate how the barrier acts at a molecular level during disease.’
Natural degeneration, ageing and lifestyle

Ageing
Why do some people suffer from depression and memory loss as they age, whereas others stay well for the whole of their lives?
The Neurobiology of Ageing group, part of the Department of Psychiatry, examine the effect of genes and life history on ageing, using neuropsychology and neuroimaging techniques as part of large scale epidemiological and experimental medicine studies.
Epidemiology:
The scientific study of the spread and control of diseases
Brain health can be affected by a wide range of neurological and psychiatric disorders, such as dementia, Parkinson’s, stroke, depression, schizophrenia and autism. Due to increased longevity, brain health related diseases are expected to increase in the coming decades, worldwide.
The Heart and Brain Ageing Group, led by Associate Professor Sana Suri, is based in the Department of Psychiatry and the Wellcome Centre for Integrative Neuroimaging at the University of Oxford. The group combines MRI and ultrasound imaging to investigate how the structure, blood supply and function of brain relate to risk and resilience for dementia.
The researchers use population level neuroimaging cohorts, such as the UK Biobank and the European Lifebrain Project, to examine the interaction of lifestyle and genetic risk on cognitive decline, ultimately hoping that by understanding the link between cardiovascular and brain health they can identify both how and when in the lifespan preventative interventions for dementia may be most effective.
‘I am using a new brain scanning technique to understand how and at what stage poor cardiovascular health can affect how we regulate the blood supply to the brain and how this in turn affects memory.’
Oxford Dementia and Ageing Research (OxDARE) is a collaborative research effort championing Oxford’s work in this area.
OxDARE provides a network for researchers and clinicians, many of whom are involved in the Older Adults and Dementia research theme, led by the Department of Psychiatry’s Professor Clare Mackay and part of the NIHR Oxford Health Biomedical Research Centre.
OxDARE research is conducted in a variety of settings, including through the Department of Psychiatry, the Clinical Research Facility, Oxford Centre for Human Brain Activity, the Wellcome Centre for Integrative Neuroimaging (WIN) and the NIHR Clinical Research Network.
The project also has a strong emphasis on public engagement, aimed at inspiring the target audience of mid-to-later life adults with and without cognitive problems to take part in dementia prevention and brain health research.
Lifestyle and risk factors for cognitive decline
The Lancet 2020 commission highlighted that there are 12 risk factors which can be potentially modified to prevent or slow the progression of dementia. These are lower levels of education, hypertension, obesity, alcohol, traumatic brain injury (TBI), hearing loss, smoking, depression, physical inactivity, social isolation, diabetes and air pollution.
Oxford’s Modifying Dementia Risk group, from the Department of Psychiatry, investigates the impact of these 12 risk factors on later life dementia and cognitive decline using large-scale population data resources. The group is led by Dr Sarah Bauermeister and is supported by Dementias Platform UK.
Recent research by Dr Bauermeister into hearing loss and its impacts on the progress of dementia in later life has shown that hearing loss is not only a risk factor for dementia but can have knock-on effects leading to some other problems including depression, a lack of exercise and obesity.
‘Being deaf can leave you socially isolated and not participating in activities. If you don’t go out of the house your world shrinks and this can have an indirect effect on cognition.’
A collaborative team including Oxford found that having higher levels of Omega-3 fatty acids in your body could boost the effect of vitamin B supplements in slowing mental decline in older people.
The researchers, including Emeritus Professor David Smith from the Department of Pharmacology, studied more than 250 people with mild cognitive impairment (MCI) in Oxford.
MCI is when brain function is below what is normally expected for a person’s age but is not significant enough to interfere with daily life. While it is not as serious as dementia, if untreated it often progresses to become dementia.
‘The next stage will be to see whether providing a combination of B vitamins and Omega-3 supplements can slow the conversion from MCI to Alzheimer's disease. This would be an important step in the prevention of Alzheimer's disease.’

Neurodegenerative diseases
Alzheimer’s disease
Alzheimer’s disease is the most common age-related neurodegenerative disease and cause of dementia, estimated to affect close to 50 million people in 2015 worldwide, with cases predicted to almost double every 20 years.
Alzheimer’s disease accounts for an estimated
60% to 80%
On World Alzheimer's Day 2022, Alzheimer's Research UK announced £420K of funding support for pioneering dementia research at the Oxford Parkinson's Disease Centre, part of the Department of Physiology, Anatomy and Genetics.
The funding is allowing Senior Postdoctoral Research Scientist Dr Becky Carlyle and her team to investigate ways to boost resilience to Alzheimer’s and reveal potential targets for new drugs that could help slow the progression of the disease.
‘Thanks to this new funding, we will be closer to understanding a key feature of Alzheimer’s, designing treatments to increase resilience in those at risk, and helping limit the impact of this devastating disease.’
Oxford researchers are undertaking innovative research with the aim of developing new drugs and treatments for Alzheimer’s disease and working to improve diagnostic methods.
Oxford Brain Diagnostics, a spinout from Oxford University, was launched in 2019 to deliver a new method for diagnosing Alzheimer’s disease from MRI scans.
The spinout was co-founded by Professor Mark Jenkinson from the Nuffield Department of Clinical Neurosciences, and in 2020 the US Food and Drug Administration (FDA) awarded its Breakthrough Device Designation to Oxford Brain Diagnostics’ Cortical Disarray Measurement (CDM®) Software Device for evaluating adults at risk of Alzheimer’s disease.
‘I am really looking forward to pushing the boundaries of the science behind our technique and exploring how it can help in the treatment and management of Alzheimer’s disease.’
Parkinson’s disease
Parkinson’s disease is a progressive illness caused by a loss of dopamine-producing neurons in the brain.
There are over 40 symptoms of Parkinson’s, which start to appear when the brain can’t make enough dopamine to control movement properly. The three main symptoms of Parkinson's are a tremor (shaking), slowness of movement and rigidity (muscle stiffness).
The Oxford Parkinson's Disease Centre (OPDC), part of the Department of Physiology, Anatomy and Genetics, is a unique multidisciplinary research program.
The OPDC was established in 2010 and brings together internationally renowned scientists who work on the genetics of Parkinson’s, the generation of cell and animal models and the wiring of brain circuits which control movement, with clinical experts in the diagnosis and treatment of Parkinson’s.
The centre works to understand the earliest events in the development of Parkinson’s with an ultimate view to target the molecular mechanisms of disease with neuroprotective therapies to prevent disease onset or delay progression.
Researchers at OPDC, led by Principal Investigators Professor Michele Hu and Professor Richard Wade-Martins, are building on our increasing knowledge of disease mechanisms in Parkinson’s to develop research aimed at changing how people with Parkinson’s are treated, focussing directly on what matters most to individuals living with Parkinson’s worldwide and identifying new therapeutic targets.
Senior research fellow Dr Charmaine Lang was recently awarded the first jointly funded Senior Research Fellowship from Parkinson’s UK and Rosetrees Trust. With this award, Dr Lang will develop complex new induced pluripotent stem cell (iPSC) models that target the interaction between dopamine neurons and astrocytes in the brain and how these fail in the context of Parkinson's.
‘I hope this work will hold significant long-term value for the wider research community and will generate much needed data surrounding the mechanistic understanding of dopamine neuron and astrocyte communication and support in Parkinson’s.’
Motor Neurone Disease
Motor Neurone Disease (MND) describes a group of conditions that affect the motor nerves and central nervous system.
They are progressive, degenerative neurological conditions that lead to muscle wasting, weakness and changes in muscle tone. Amyotrophic lateral sclerosis (ALS) is the most common form of Motor Neurone Disease.
MND is the
third most common
form of neurodegenerative disease after Alzheimer’s and Parkinson’s
Research from the Oxford Motor Neuron Disease Centre, part of the Nuffield Department of Clinical Neurosciences, focuses on the early stages of the disease when it is believed there is the most chance of applying effective treatments.
Led by Professor Kevin Talbot, the group aims to identify the earliest changes which occur in the disease and apply protective therapies before the onset of significant disability in those at risk and those already living with ALS.
About 10% of patients with MND have a genetic mutation and each of their close relatives (parents, siblings and children) will have a 50% chance of carrying the gene that leads to MND.
Funding from the Alan Davidson Foundation supports the work of Professor Talbot and his group to deliver an innovative research project using the genetic causes of MND to develop approaches to early diagnosis.
The research will sign up 300–400 at-risk individuals, who will be carefully monitored to enable the team to pick up the very earliest signals of the disease, with the aim of producing a blood test that could be used in general practice to screen for the silent damage occurring in the early phase of MND.
‘This pioneering new project aims to understand the very earliest changes that occur, before physical symptoms progress. In the longer term it will contribute towards our aim of making MND a preventable condition.’
Cerebellar ataxia
Ataxias collectively refer to a group of different neurological disorders that can affect coordination, balance and speech.
Oxford’s Cerebellar Disease Group, part of the Nuffield Department of Clinical Neurosciences, is led by Professor Esther Becker and focuses on understanding the genes and pathways behind cerebellar diseases, particularly cerebellar ataxia.
The group’s work with Professor Andrea Németh, also from the Nuffield Department of Clinical Neurosciences, and her team identified the first dominant gene mutations in Spinocerebellar ataxia type 41 (SCA41) and 44 (SCA44).
Spinocerebellar ataxias are a group of diseases that are caused by degenerative changes in the cerebellum. There are many different types of spinocerebellar ataxia with unique symptoms, however, in general, all are characterized by problems with movement that tend to get worse over time.
In a collaborative paper, the researchers identified, for the first time, dominant mutations in the gene GRM1 that cause distinct disease symptoms, opening opportunities to develop therapeutic treatments for cerebellar ataxias.
‘This is a really exciting development in understanding both neurodegenerative and neurodevelopmental cerebellar ataxia.’
Friedreich’s Ataxia, also known as FA or FRDA, is a devastating, progressive, neurological movement disorder affecting multiple organs and cell types in the body. FA affects approximately 1 in 40,000-50,000 people and onset is typically between 10 and 15 years of age.
Friedreich’s ataxia is caused by mutations in the frataxin gene. The work of the Wade-Martins Group in the Department of Physiology, Anatomy and Genetics, led by Professor Richard Wade-Martins, seeks to better understand the underlying genetic mechanisms of Friedreich’s ataxia, and develop small molecule therapies to alleviate its effects.
Friedreich’s ataxia is a priority area of research for the Oxford-Harrington Rare Disease Centre (OHC), a partnership between the University of Oxford and the Harrington Discovery Institute in Cleveland, Ohio, US.
The centre recently established the Friedreich’s Ataxia Alliance at Oxford (FA Alliance), a consortium of scientific and clinical investigators coordinated by Dr Geoffrey Denwood, from the Department of Paediatrics, committed to developing new therapies for Friedreich’s ataxia.
The FA Alliance team, including Professor Richard Wade-Martins and Dr Geoff Denwood, raising awareness for Friedreich’s ataxia.




Dementia
Dementia is an umbrella term for a range of progressive conditions that affect the brain.
Each type of dementia stops a person’s brain cells from working properly in specific areas, affecting their ability to remember, think and speak. There are over 200 subtypes of dementia, the most common being Alzheimer’s disease.
Over 50 million
people suffer from dementia worldwide, a figure that is predicted to rise to 150 million by 2050
Dementias Platform UK (DPUK) is a public-private partnership with core funding from the Medical Research Council aimed at speeding up progress in dementia research. Based at Oxford, DPUK brings together expertise from universities, charities, and pharmaceutical and technology companies in a high-trust, collaborative environment.
DPUK gives scientists access to the latest data, technologies and research opportunities to help bridge the gap between fundamental discoveries in the lab and successful trials of new treatments for dementia.
By bringing together what is known as cohort data, DPUK offers the chance for more specific drug trials that can be carried out earlier in the progression of the disease.
‘When researchers study the people for whom we have a lot of data – the people who take part in cohort studies – we are in a much stronger position to make the breakthroughs we need in the dementia treatment deadlock.’
John Gallacher is the Director of DPUK and Professor of Cognitive Health at Oxford’s Department of Psychiatry and spoke about the future of dementia research in a recent podcast.
Multiple sclerosis
Multiple sclerosis (MS) affects 2.5 million people worldwide and approximately 100,000 people between the ages of 20-40 years in the UK.
In this chronic debilitating condition the immune system attacks nerve cells resulting in symptoms including numbness, tingling, blindness and even paralysis.
Understanding MS is complicated because unlike in other diseases, the site of inflammation – the brain – is not readily accessible in living patients.
Researchers from the Universities of Oxford and Hamburg revealed a disease-causing population of immune cells, which travel to the brain in patients with MS. Using an approved treatment, which blocks transit through the blood brain barrier, they demonstrated a unique opportunity for cell targeting to prevent disease progression.
‘We were able to generate high quality data, maximising the use of precious patient samples. This allowed us to reveal novel characteristics of this population, which could be used to develop new treatments that eliminate them before they enter the brain and drive disease.’
Researchers, including Professor Lars Fugger and Dr Hayley Evans from the Oxford Centre for Neuroinflammation, followed these immune cells from the blood to the brain, utilising rare tissue samples from deceased late-stage MS patients.
Using a cutting-edge technology called spatial transcriptomics, they were able to locate the gene signatures of these cells using a detailed physical map. In this way, the researchers demonstrated that those specific immune cells were indeed localised in areas of brain damage in patients.
‘Our results suggest that the colonisation of the brain by immune cells could be an important factor in the therapeutic resistance of late-stage MS.’
Huntington’s disease
Huntington's disease is an inherited genetic condition that typically begins in mid-life. It results in movement control difficulties and dementia, and can cause significant behavioural problems. It progresses to severe disability and death over approximately 20 years.
50% risk
of children of affected individuals inheriting Huntington’s disease
Professor Andrea H Németh from the Nuffield Department of Clinical Neurosciences led the Oxford arm of a ground-breaking clinical trial for Huntington’s disease. The GENERATION HD1 trial was conducted at Oxford’s John Radcliffe Hospital, with three patients at Oxford University Hospitals NHS Foundation Trust being among the first in the world to receive a pioneering experimental treatment with the aim of lowering the amount of the disease-causing toxic protein produced in the nervous system of patients.
The GENERATION HD1 trial prematurely ended following a review of preliminary results, however a phase II of the trial will use the findings for further investigation into use of the novel treatment for Huntington’s disease.
Oxford researchers conducted a survey to determine whether brain imaging markers of tissue microstructure can detect the effect of disease progression across the preclinical stages of Huntington's disease.
The collaborative team, including Associate Professor Gwenaëlle Douaud and Professor Mark Jenkinson and demonstrated for the first time significant changes in brain structure between preclinical stages of Huntington’s disease, suggesting imaging could be used for monitoring treatment response and identifying the optimal therapeutic window of opportunity in preclinical Huntington's disease.

Brain banks and collections
Oxford Brain Bank
Oxford’s ground-breaking research into the mechanisms and causes of neurodegenerative diseases would not be possible without the use of tissue samples from donated organs.
The Oxford Brain Bank is a large collection of donated brain and spinal cord tissue that can be used for research into neurological diseases, including Parkinson's disease, Alzheimer's disease and other causes of dementia, Motor Neuron Disease, Multiple Sclerosis and ataxia, autism and brain tumours.
In an event co-hosted by the Nuffield Department of Clinical Neurosciences, brain tumour patients and carers were given the opportunity to see what clinical researchers in Oxford are doing to improve diagnosis and care.
‘These sorts of events help to demystify medicine and I hope there'll be more of them.’
Thomas Willis Brain Collection
The Thomas Willis Brain Collection contains one of the largest neuropathology collections in the UK - including brains from the previous Oxford Project to Investigate Memory and Ageing (OPITMA), led by the Nuffield Department of Clinical Neurosciences, and the ongoing Brains for Dementia Research (BDR) study.
Research projects include pathology, genetics and microstructure of ageing and dementia, vascular disease including small vessel disease, and neuropathology of movement disorders and Motor Neuron Disease. The collection is hosted by the Nuffield Department of Clinical Neurosciences’ Neuropathology facility and underpins much of the group’s research.
The collection is part of the UK Brain Banks Network, an initiative funded by the Medical Research Council.
Emeritus Professor Margaret Esiri spoke in a podcast about the pivotal role Oxford has played in neuroscience, and how the Thomas Willis Brain Collection is at the centre of research into finding out more about the underlying causes and potential treatments of neurological conditions.
Digital Brain Bank
The Wellcome Centre for Integrative Neuroimaging at the University of Oxford is host to the Digital Brain Bank, a data release platform providing open access to curated, multimodal post-mortem neuroimaging datasets.
Post-mortem MRI provides the opportunity to validate the origins of image contrast through comparisons with microscopy, and acquire high-resolution datasets to investigate structural and comparative anatomy.
Concussion Legacy Foundation UK
The Concussion Legacy Project is a brain bank for research on Chronic Traumatic Encephalopathy (CTE) and other consequences of brain trauma.
Professor Gabriele DeLuca from the Nuffield Department of Clinical Neurosciences leads the Concussion Legacy Project in the UK.
‘Brain donation will allow us to better understand the complexities of CTE so that we can develop tailored interventions and treatments to prevent its devastating consequences.’
In 2022, the Oxford University Men’s Rugby team pledged to donate their brains to the Concussion Legacy Project, to support research that will help change the future of neurodegenerative disease in sport.