Mental health and the world around us

From the stresses of climate change to economic inequalities, researchers at the University of Oxford are uncovering how the world around us can impact our mental health.
Oxford’s experts are using virtual reality simulations to treat serious mental health conditions and examining the role our social networks and communities play in supporting mental wellbeing.
Climates and climate change
Researchers at the Nuffield Department of Medicine have investigated the link between mental disorders and climate, finding it to be positively associated with temperature in cool to cold climatic regions, but the association in warmer regions was less clear.
The study looked at the short-term association between temperatures and mental disorder hospitalisations in a subtropical city with a mean annual temperature over 21°C.
The results found a positive temperature–mental-disorder association in a warm subtropical region, most prominent among older people.
‘If radical action to reduce emissions isn’t taken in the next decade or so, many of today’s schoolchildren could live in a world that’s 3℃ or 4℃ hotter by the time they enter their later years. Their working lives would be defined by routine weather extremes, widespread crop failures and catastrophic sea level rise.’
A number of researchers, including the Department of Psychiatry’s Professor Charles Newton, contributed to a study examining the impacts of a changing climate on disease and mental health.
The study noted that the associated global warming and humidification, increases in the severity and frequency of extreme climate events, increased ranges of vector-borne diseases, and the consequent social and economic stresses and disruption will have major negative consequences on many aspects of health care, including mental health.
Heatwaves and mental health conditions
Oxford’s experts are investigating the huge impact of heatwaves on our physical and mental health.
Recent studies suggest at least a 10% rise in hospital emergency room visits on days when temperatures reach or exceed the top 5% of the normal temperature range for a given location.
Heatwaves – as well as other weather events such as floods and fires – have been linked to a rise in depressive symptoms in people with depression, and a rise in anxiety symptoms in those with generalised anxiety disorder – a disorder where people feel anxious most of the time.
There is also a link between daily high temperature and suicide and suicide attempts. And, roughly speaking, for every 1℃ increase in monthly average temperature, mental health-related deaths increase by 2.2%.
Spikes in relative humidity and temperature also result in a higher occurrence of suicide, manic episodes in people with bipolar disorder, and can reduce the effectiveness of drugs used to treat psychiatric illness.
Dr Laurence Wainwright, from Oxford’s Smith School of Enterprise and the Environment, writes in an article co-authored by Dr Eileen Neumann from the University of Zurich that heat can also affect the mental health and ability to think and reason of people without a mental health disorder, as areas of the brain responsible for framing and solving complex cognitive tasks are impaired by heat stress.
There is also strong evidence linking extreme heat with a rise in violent crime, and by 2090, it is estimated that climate change could be responsible for up to a 5% increase in all crime categories, globally.
Eco-anxiety
The School of Geography and the Environment is examining how students studying in the fields of conservation and the environment can be particularly vulnerable to the mental health impacts of climate stress.
Eco-anxiety:
Extreme worry about current and future harm to the environment caused by human activity and climate change
MSc student Raphaella Mascia describes the unique challenges faced by students in Environment and Conservation, and the issues related to mental health, eco-stress, anxiety and grief in an article published for Earth Day 2023.
‘Mental health is a complex subject, and eco-stress even more so as it has only just come to light in the last decade. Although we have much much further to go towards destigmatising and understanding student mental health in the environmental and conservation field, we have a place to begin.’
Raphaella also looks at how a lack of work opportunities impact the mental health of students in these fields, and the significant role of community and educators in reducing these stressors.



Virtual reality environments


Virtual reality has been used to treat a number of psychological disorders, and it has several major advantages over exposing patients to a real-life situation.
Peoples’ minds and bodies react as they would in the real world but, because the patients know the situation is artificial, they are much more confident about trying out different psychological techniques.
They can gradually build up the difficulty level of the situations so that learning can be made at a manageable pace.
Dr Marieke Martens, a researcher at the Department of Psychiatry, investigates the impact of the catechol-O-methyltransferase’s (COMT) gene on brain functions relevant to psychiatric illness.
Her research looks at how the links between dopamine, COMT, and memory are altered by environmental factors like stress.
To measure the physiology of stress responses and potential implications for psychiatric disorders, Dr Martens performed a study using a virtual reality (VR) environment, examining the stress response in 28 healthy men exposed either to stressful VR simulations or a control.
Compared to participants in the control environment, those in the stressful environment had increases in skin conductance, pulse and subjective stress and anxiety ratings, altered heart rate variability, and a delayed rise in cortisol.
About 1-2% of the population has severe paranoia, typically as a central feature of mental health disorders such as schizophrenia.
A research team led by Professor Daniel Freeman from Oxford’s Department of Psychiatry, with funding from the Medical Research Council, wanted to test how virtual reality can help treat severe paranoia by allowing people to face situations that they fear.
Thirty patients attending treatment services at Oxford Health NHS Foundation Trust took part in the study. All the patients went into virtual reality simulations with increasing numbers of computer characters, a situation that would normally make these patients anxious. Staying in these situations allowed the patients to learn that the situations they feared, such as a crowded lift or a train ride, were actually safe.
‘Paranoia all too often leads to isolation, unhappiness, and profound distress. But the exceptionally positive immediate results for the patients in this study show a new route forward in treatment. In just a thirty-minute session, those who used the right psychological techniques showed major reductions in paranoia.’
The spinout company OxfordVR came from the work of Professor Freeman’s lab.
OxfordVR use virtual reality for immersive technology to enable greater access to cost-effective and high-quality therapy for treating mental health conditions, specifically psychosis.
Their VR interventions create powerful simulations of the scenarios in which psychological difficulties occur and have been proven to be successful in reducing patients’ fears by up to 68%.
The gameChange VR program was developed by a multi-partner team of university, health and industry experts including OxfordVR, researchers at the University of Oxford and Oxford Health NHS Foundation Trust.
The largest ever clinical trial of VR for mental health, gameChange VR is a landmark psychological therapy targeting a problem that is common in people diagnosed with psychosis: intense fears about being outside in everyday situations.
Funded by the National Institute for Health and Care Research (NIHR), the technology is designed to treat this agoraphobia and help patients re-engage with day-to-day activities, taking them from a housebound existence to life back in the world outside.
‘Using today’s affordable and easy-to-use consumer VR equipment, we think gameChange will lead a transformation in the digital provision of evidence-based psychological therapy, with deployment at scale for treatments that really work.’

Social environments
Social determinants of mental health are wide-ranging and can be linked to poverty; material deprivation; unemployment; poor housing, including exposure to hazardous or noisy or unsafe homes; gender disadvantage, poor educational opportunities, violence, social and cultural inequalities in opportunities; and exposures to adversity, including discrimination, stigma, and prejudice.
The importance of community
Humans are intensely social and benefit psychologically and physically from social interaction. The tighter we are embedded in a network of friends, for example, the less likely we are to become ill and the higher our rates of survival.
People who belong to more groups, such as sports clubs, church, or hobby groups, have been found to reduce their risk of future depression by almost 25%.
A study co-authored by Associate Professor Danilo Bzdok (McGill University and Mila Quebec Artificial Intelligence Institute) and Emeritus Professor Robin Dunbar of Oxford’s Department of Experimental Psychology explored the wide-ranging, negative consequences that social isolation has on our psychological wellbeing and physical health, including decreased life span.
The results revealed the severe impact loneliness can have, including reducing resilience to physical and mental disease, increasing the likelihood of perceiving social cues in a negative manner, escalating morbidity and mortality, and, in older people, precipitating the onset of dementia, such as Alzheimer’s disease.
People who feel a stronger sense of cohesion within their neighbourhood have higher levels of mental wellbeing, independent of social class, income, presence of limiting illness or disability, mobility problems, and perceived social support.
Oxford research has demonstrated the relationship between individuals' social, cultural and community engagement and the effect these activities have both on the prevention and management of mental illness.
Oxford researchers found evidence that the quality and size of our social networks can impact how we experience stress and pain. Dr Katerina Johnson of the Department of Experimental Psychology tested the theory that social interactions trigger positive emotions when endorphins bind to opioid receptors in the brain and found that people who could endure a pain test for longer also tended to have larger social networks.
‘Studies suggest that the quantity and quality of our social relationships affect our physical and mental health and may even be a factor determining how long we live. Therefore, understanding why individuals have different social networks sizes and the possible neurobiological mechanisms involved is an important research topic.’





Social activities
One in five people will develop major depression at some point in their life. The total annual cost of depression in the UK is about £8 billion.
Research from Oxford’s Department of Psychiatry shows that healthy mood regulation, such as choosing activities to cheer yourself up, was impaired during periods of social isolation and lockdown due to COVID-19, potentially resulting in depression.
The researchers, including Professor Guy Goodwin and Dr Maxime Taquet, suggest that supporting natural mood regulation could be a new target for treating and reducing depression.
This research is supported by the NIHR Oxford Health Biomedical Research Centre and the Royal College of Psychiatrists.
‘By training people to increase their own mood homeostasis, how someone naturally regulates their mood via their choices of activities, we might be able to prevent or better treat depression.’
Dr Anne Ferrey, a Health Psychology researcher at the Nuffield Department of Primary Care Health Sciences, co-led an innovative public engagement project to investigate whether yarn-based crafting can improve health and wellbeing.
The Yarnfulness Project was awarded Oxford University Public Engagement Seed Funding and aims to engage with local and online communities who practice yarn-based crafts, in order to understand their opinions of mindfulness practice, as well as the widely reported benefits of yarn-based craft, based on the idea that focusing on a creative task can break the loop of negative thought that is common in depression or anxiety.
‘It does make intuitive sense that enjoyable leisure activities might improve wellbeing, and even that there might be something specific to creative activities, like knitting, that could provide a particular boost.’
Research from the Department of Experimental Psychology shows that the more often people eat with others, the more likely they are to feel happy and satisfied with their lives.
Using data from a national survey by The Big Lunch - an idea from the Eden Project made possible by the Big Lottery Fund - Professor Robin Dunbar looked at the link between social eating and an individual’s happiness, the number of friends they have, their connection to their community, and overall satisfaction with life, and found that communal eating increases social bonding and feelings of wellbeing, and enhances one’s sense of contentedness and embedding within the community.
‘In these increasingly fraught times, when community cohesion is ever more important, making time for and joining in communal meals is perhaps the single most important thing we can do – both for our own health and wellbeing and for that of the wider community.’

Socio-economics
Socio-economics and mental health
Research into social determinants of health and wellbeing seemed to tell a simple story: the poorer you are, or the lower your class, the worse your health and well-being is likely to be.
Researchers from the Oxford Martin School undertook research on social class and psychological well-being, and found that that employment status is another consideration when measuring psychological wellbeing. They found that social class is a key factor in determining access to the labour market, which has clear implications for psychological health.
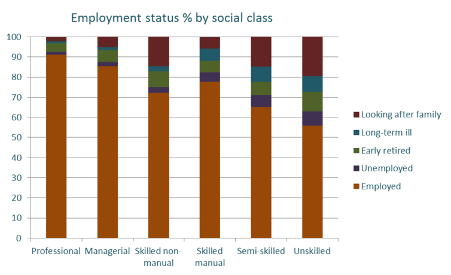
The chances of being in the labour market are far higher in the higher social classes (Health Survey for England)
The chances of being in the labour market are far higher in the higher social classes (Health Survey for England)
Research from Oxford’s Department of Sociology examined the impact of widening economic inequality on mental health as a result of the Covid-19 pandemic.
Dr Dirk Witteveen, joint author of the study with Dr Eva Velthorst of New York’s Icahn School of Medicine, found that socio-economic inequalities were exacerbated during the lockdown. The most vulnerable members of the labour market were the most affected, suffering more income and job loss, and as a result suffering ‘substantial’ mental health consequences.
‘We found that experiencing any of these COVID-19-induced economic hardships is predictive of higher probability of depression complaints and health anxiety. Moreover, this probability appeared to be about twice as great for individuals employed in lower prestige-ranked jobs compared with people in middle- and higher-ranked jobs.’
The Co-SPACE (COVID-19 Supporting Parents, Adolescents, and Children in Epidemics) study is led by experts at the University of Oxford, and was set up to understand how families have coped throughout the COVID-19 pandemic, and what parents can do to support their children’s mental health.
This research is funded by the Economic and Social Research Council (ESRC) as part of the UK Research and Innovation (UKRI)’s rapid response to COVID-19 and the Westminster Foundation, and supported by the NIHR Oxford Health Biomedical Research Centre, the Oxford and Thames Valley NIHR Applied Research Consortium and the UKRI Emerging Minds Network Plus.
A recent Co-SPACE report, co-led by Professor Cathy Creswell from the Department of Experimental Psychology, found that children from low-income backgrounds showed elevated mental health difficulties throughout lockdown.
Parents and carers from low-income households reported that their children (aged 4 to 16 years) had higher levels of emotional difficulties, such as feeling unhappy, worried, being clingy and experiencing physical symptoms associated with worry than those from higher income households.
Their children were also more fidgety and restless and had greater difficulty paying attention. Those with younger, primary school aged children also reported that their children were experiencing higher levels of behavioural difficulties, including temper tantrums, arguments, and not doing what they were being asked to do by adults than those from higher income households.
‘These findings highlight not only the huge variation in how children and young people have been coping throughout the pandemic but also how pre-existing vulnerabilities associated with inequality have continued during the crisis.’
Oxford’s Mind & Behaviour Research Group brings together economists, psychiatrists, and psychologists as part of the Centre for the Study of African Economies. Researchers investigate the psychological impact of living in poverty and using their findings to improve policy programmes.
Suicide is a pressing public health concern, causing 800,000 deaths per year globally, and suicidal behaviour is one of the leading causes of death for people with severe mental illness.
A collaborative study including Dr Lukas Hensel examined whether poverty alleviation programmes can decrease suicides, as well as whether they can alleviate the effects of droughts on suicides.
Poverty alleviation programmes in the shape of conditional and unconditional cash transfer programs have been implemented in many developing countries. The team studied whether the Program Keluarga Harapan (PKH) conditional cash transfer program in Indonesia reduced suicide rates.
The study revealed the PKH program reduced the suicide rate by 18%, an estimate of about 1,065 suicides. The researchers also found that droughts affect suicides, with one standard deviation decrease in rainfall increases the suicide rate by 0.8 suicides per 100,000 population.
This relationship disappears in sub-districts that receive the PKH program, suggesting that poverty alleviations programmes do save lives by preventing suicides and alleviating mental health disorders such as depression.
‘Globally, an estimated 264 million individuals in low- and middle-income countries suffer from depression. While there is growing awareness that mental health conditions in poor countries have economic and social effects, in many developing countries less than 10% of common mental health disorders are treated.’
Protecting the mental health of children in low-resource settings
Researchers from Oxford’s Department of Social Policy and Intervention are developing resources to prevent violence in low-resource settings.
Dr Jamie Lachman and Professor Lucie Cluver lead the award-winning Parenting for Lifelong Health (PLH) initiative, developed in collaboration with the World Health Organisation and UNICEF, as well as academic colleagues from South Africa and the United Kingdom.
Recent knowledge about the prevalence of child maltreatment and other childhood adversities, and about the links between childhood adversities, poor parenting, and their serious and life-long consequences, has resulted in multiple calls for innovative and concerted strategies to reduce them.
Successful programmes in high-income countries are very often too expensive for low- and middle-income countries and not always culturally appropriate.
Hence, there have been no widely available parenting support programmes that are evidence-based, culturally appropriate, and affordable for low-resource settings, where the need is the greatest.
4 million +
families reached in Pakistan
Parenting for Lifelong Health, developed and tested by Dr Jamie Lachman, Professor Lucie Cluver, and Professor Frances Gardner, along with other UN and academic colleagues, is a suite of open access, non-commercialised programmes with a key goal of preventing child maltreatment and involvement in other forms of violence.
Evidence shows that preventing child maltreatment and later violence can also result in important long-term physical and mental health and socio-occupational benefits as children become adults and parents themselves.
The programmes are currently being delivered in 40 low- and middle-income countries across Sub-Saharan Africa, South-eastern Europe, Southeast Asia, and the Caribbean.
11.6 million +
families reached in Ukraine
This project has led to several studies to further develop the evidence base for these interventions, including the RISE project led by Dr Lachman, which aims to determine the most effective and cost-effective version of the PLH programme in order to prevent child mental health problems in three Eastern European countries: Northern Macedonia, the Republic of Moldova, and Romania.
Professor Cluver and Dr Isang Awah were among a group of Oxford experts who worked with Oxford University’s Ukrainian community to create a package of free, easy-to-use advice for families affected by the war.
‘These will help families to cope with stress, make safety plans for their children, support children through fear and danger, and build children’s resilience to crisis’
2023 earthquakes in Turkey and Syria
The collegiate University offers its deepest sympathy and support to any student or staff member affected by the tragic events in Turkey and Syria.
On Thursday 9 February 2023, the Pro-Vice-Chancellor for People & Digital and the Pro-Vice-Chancellor for Education wrote to all University staff and students with Turkish or Syrian nationality offering support and practical advice.
Information, advice and support for staff and students impacted
Having reached over 15 million families in Ukraine and Pakistan, the Parenting for Lifelong Health team, led by Professor Cluver and Dr Lachman, have again worked with the WHO, UNICEF, UNHCR and UNODC to create rapidly shareable social media assets and resources.
Based on 15 Oxford-University led randomised control trials of parenting interventions, the assets and resources include invaluable tips for parents and caregivers in Turkey and Syria.




Geopolitics

Natural and man-made disasters carry with them major burdens and very often the focus is on immediate survival and management of resulting infectious diseases. The impact of disasters directly and indirectly on the wellbeing and mental health of those affected often gets ignored. The reasons are often stigma and lack of attention to mental health consequences.
Mental health is likely to be affected both directly and indirectly as a result of disasters and also likely to be influenced by ongoing factors such as poor housing, overcrowding, and other social determinants.
Brexit and mental health
A study led by senior researchers at the Nuffield Department of Primary Care Health Sciences, in collaboration with researchers from Bocconi University, Italy and Universitat Pompeu Fabra, Spain, undertook a study to analyse the changes in mental health in the UK that occurred as a result of the 2016 referendum on UK membership of the EU (Brexit).
Research Fellow Joan Madia and Dr Catia Nicodemo contributed to the study, which used data from the UK Household Longitudinal Study (UKHLS), a panel data survey consisting of 40,000 households from the UK, to compare the levels of self-reported mental distress, mental functioning, and life satisfaction before and after the referendum.
Findings from the study indicate an overall deterioration in mental health in the two years after the referendum of 2016. Young adults (aged 31–46), men, natives, and highly educated individuals, living in areas where more than 50% of the voters were in favour of remaining in the EU, were significantly more affected by the results of the referendum than any other groups.
The study provides further evidence on the decline in average mental health as a consequence of the Brexit referendum and the economic uncertainty associated with it, and also shows that its effects are long-lasting in the population.
Olympic legacy
Professor Trish Greenhalgh from the Nuffield Department of Primary Care Health Sciences contributed to a study examining the effects of the London 2012 Olympics and related urban regeneration on physical and mental health.
The qualitative study found that residents generally welcomed the unexpected chance to live in a cleaner, safer and more unified environment, and that the Games temporarily alleviated certain stressors in the social and physical environment. Overall, the Games lessened participants’ sense of social exclusion and appeared to generate a sense of inclusion and respite, even if this was only temporary.



