Dementia

Dementia is a devastating condition affecting around 50 million people worldwide, a figure predicted to rise to 152 million by 2050.
Oxford experts are undertaking urgent research to better understand the impacts of dementia, its possible causes and how it relates to our overall brain health. They are examining what factors can increase our risk of the diseases that cause dementia, so that this knowledge can ultimately be translated into preventative strategies.
Dementia can be particularly challenging to study, and our researchers are continually interpreting the evidence to answer the question we all want to know: how can we best protect ourselves against dementia?
What is dementia?

The term ‘dementia’ describes a related group of symptoms caused by a progressive decline in brain function. These symptoms can include memory loss, problems with language, confusion, changes in mood and agitated or aggressive behaviour.
Many different diseases cause dementia, the most common being Alzheimer’s disease, which makes up 60% of UK dementia diagnoses.
152 million people
are predicted to be affected by dementia by 2050
Someone in the UK develops dementia every three minutes, with an estimated third of cases undiagnosed, and it can take up to ten years from the first symptoms for an individual to be diagnosed with dementia.
Find out more about Oxford’s research on the various diseases that cause dementia.
Risk factors for dementia
Cognitive decline and ageing
Cognitive decline typically precedes dementia and can affect individuals in very different ways, depending on the pathology of the underlying disease and which region of the brain is affected.
In a pioneering dementia study that included researchers from the Department of Psychiatry, people over the age of 50 were invited by the NHS to join a European-wide study looking at long term risks for developing Alzheimer’s dementia.
Participants were asked to take part in physical and cognitive tests so researchers could study changes in people who do and do not develop the condition.
The ongoing study is part of The European Prevention of Alzheimer’s Dementia (EPAD) Project and is supported by the NIHR.
‘EPAD is a hugely supported, European-wide initiative that will make a massive difference to the understanding and management of Alzheimer’s disease. Its broad assessments and pioneering design could mean this study really changes how we defeat this global disease.’
Cardiovascular risk factors
Nearly a third of dementia cases could be prevented by modifying our lifestyle, in particular our cardiovascular health.
Oxford researchers are working to understand the links between cardiovascular and brain health to identify how lifespan interventions for dementia may be most effective.
The Heart and Brain Ageing Group, based in the Department of Psychiatry and Wellcome Centre for Integrative Neuroimaging, investigates this heart-brain link in detail, by studying how the health of our heart and large blood vessels affect the brain and memory as we grow older.
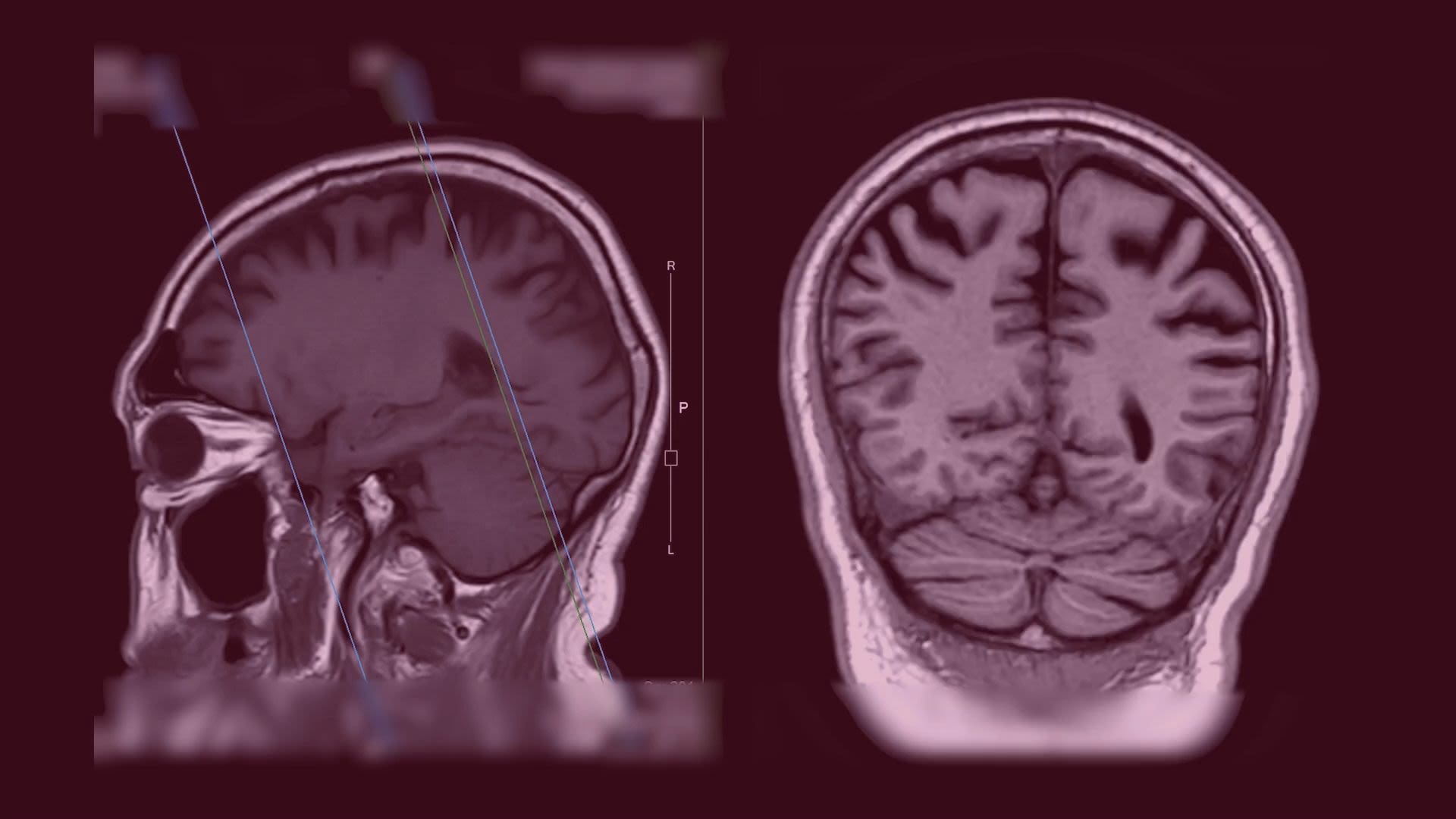
Led by Associate Professor Sana Suri, the group combines multi-modal magnetic resonance imaging (MRI) and ultrasound imaging to investigate how the structure, blood supply and function of the brain relate to risk and resilience for dementia.
Associate Professor Suri and her team work with participants from the UK Whitehall II Imaging cohort, a group of people who have already had annual heart health tests since they were 40 years old.
‘I am using a new brain scanning technique to understand how and at what stage poor cardiovascular health can affect how we regulate the blood supply to the brain and how this in turn affects memory.’
In a study conducted with University College London, researchers measured aortic stiffness in 542 older adults from the Whitehall II Study.
The body’s largest artery (the aorta) gets stiffer with age, and the study found that faster aortic stiffening in mid-life to older age was linked to markers of poorer brain health.
‘Reduced connectivity between different brain regions is an early marker of neurodegenerative diseases such as Alzheimer's disease, and preventing these changes by reducing or slowing down the stiffening of our body's large blood vessels may be one way to maintain brain health and memory as we grow older.’
The Whitehall Imaging sub-study combines MRI brain imaging with detailed clinical and psychological material acquired over a 30 year period.
Professor Klaus Ebmeier, from the Department of Psychiatry, outlines research findings from the study and discusses factors in mid-life that affect brain structure in later-life.
In a large-scale study, researchers from the Nuffield Department of Clinical Neurosciences found that having multiple conditions that affect the heart is linked to a greater risk of dementia than having high genetic risk.
Conducted with the University of Exeter, the study is among the largest ever to examine the link between several heart-related conditions and dementia, and one of the few to look at the complex issue of multiple health conditions.
The team, including Dr Xin You Tai, looked at data from more than 200,000 people from the UK Biobank, identifying those who had been diagnosed with diabetes, stroke, or a heart attack, or any combination of the three, and those who went on to develop dementia.
The researchers found that the more of these three conditions a person had, the higher their risk of dementia.
‘We found that having such heart-related conditions is linked to dementia risk to a greater extent than genetic risk. So whatever genetic risk you were born with, you can potentially make a big impact on reducing risk of dementia by looking after heart and metabolic health throughout life.’
Professor Kazem Rahimi from the Nuffield Department of Women's & Reproductive Health was lead author in a study that found heightened blood pressure increases the risk of developing vascular dementia by 62%.
Vascular dementia:
Vascular dementia affects around 9.3 million people globally and is caused by reduced blood supply to the brain due to diseased blood vessels
Analysing the medical records of 4.28 million people in the UK, the study also found that high blood pressure was still a risk factor even after adjusting for the presence of stroke, the leading cause of vascular dementia.
‘Our results suggest that lowering blood pressure, either by exercise, diet or blood pressure lowering drugs, could reduce the risk of vascular dementia.’





Multimorbidity & hearing loss
Research led by Oxford Population Health has found that living with two or more health conditions is associated with a 63% increased risk of developing dementia.
The researchers, including Dr Thomas Littlejohns, used data from more than 200,000 UK Biobank participants to investigate how a diverse range of individual health conditions increase the risk of dementia, including high blood pressure, diabetes, stroke, depression and hearing impairment.
They found that having multiple conditions, or multimorbidity, was associated with a 63% increased risk of developing dementia over a period of 15 years.
‘When considering how to reduce the risk of dementia, our findings suggest that focusing on multiple, rather than single, health conditions is important. More work needs to be done to look into whether these associations are causal, but even if they aren’t, then having multiple conditions might be an important early warning sign for a person’s risk of dementia.’
Another Oxford Population Health study using UK Biobank data found that difficulty hearing spoken conversations is associated with up to 91% increased risk of dementia.
With hearing impairment affecting up to 1.5 billion people worldwide, their research suggests there is growing evidence that this could increase the risk of dementia.
‘There is growing evidence that developing dementia is not inevitable and that the risk could be reduced by treating pre-existing conditions. Whilst preliminary, these results suggest speech-in-noise hearing impairment could represent a promising target for dementia prevention.’
Research from the Department of Psychiatry and Dementias Platform UK found that hearing loss increased the risk of mild cognitive impairment (MCI), a precursor to dementia, but this increased risk is not present in people who wear hearing aids.
The study, led by Dr Sarah Bauermeister, was the first to investigate the link between hearing aids, cognitive decline, and progression to MCI in cognitively healthy individuals.
‘Our findings provide compelling evidence in support of hearing aid use, but we now need clinical trials to objectively measure hearing aid use in the context of dementia to establish a causal link. We also encourage other researchers to incorporate hearing aid usage as a confounding factor when analysing changes in cognitive function. ’
Dr Bauermeister’s research into hearing loss and its impacts on the progress of dementia in later life featured in extensive media coverage of a Brain Health Check-In tool created by Alzheimer's Research UK.
Dr Bauermeister noted that hearing loss is not only a risk factor for dementia but can have knock-on effects leading to other conditions including depression, a lack of exercise and obesity.
‘Being deaf can leave you socially isolated and not participating in activities. If you don’t go out of the house your world shrinks and this can have an indirect effect on cognition.’
Dr Bauermeister has called for people to get regular hearing checks throughout their life to spot any auditory decline which may indicate an increased dementia risk.
Hearing loss, she says, is the single biggest factor which can increase a person’s risk
‘Regular hearing checks are very important, and this is across the lifespan, so that it’s normalised to have a hearing check, whether you are 30 or 40 years old. If we normalise hearing checks, it will normalise the wearing of a hearing aid and the stigma will then be reduced.’

Modifying risk
Lifestyle factors
Dementia and other degenerative diseases of the brain often develop slowly over many years before they are diagnosed, and this can make it difficult to study lifestyle factors which may be linked to their development.
The Modifying Dementia Risk group, part of the Department of Psychiatry, investigates the impact of the 12 risk factors on later life dementia and cognitive decline, as identified in the Lancet 2020 commission.
The group, led by Dr Sarah Bauermeister and supported by Dementias Platform UK and Alzheimer's Research UK, uses largescale population datasets to determine the importance and significance of these risk factors.
40%
of worldwide dementia diagnoses are thought to be caused by 12 modifiable lifestyle factors
The risk factors identified which can be potentially modified to prevent or slow the progression of dementia are lack of education, hypertension, obesity, alcohol, traumatic brain injury (TBI), hearing loss, smoking, depression, physical inactivity, social isolation, diabetes and air pollution.

Our researchers suggest adopting eight healthy behaviours that look after your brain, even if you already have a diagnosis of dementia.
1. Eat a diet low in cholesterol, salt and sugar
There is a collection of evidence that suggests a Mediterranean diet – one rich in vegetables, fresh fruit, grains, unsaturated fat, olive oil, fish and beans – is good for brain health.
This is partly because this type of diet is low in saturated fat and sugar, so reduces the risk of conditions like diabetes and obesity that are in turn risk factors for dementia.
2. Get plenty of exercise
Exercising can lower your risk of developing dementia by helping to keep cholesterol and obesity at bay, as well as keeping your blood vessels and heart healthy.
Evidence shows that exercise reduces decline in thinking and memory skills in people with Alzheimer's disease, and improves their physical and mental wellbeing.
3. Don't smoke cigarettes
There is a long-established link between smoking and dementia: smoking is a risk factor for dementia and can also speed up the progression of dementia via the mini-strokes that underpin vascular dementia.
Therefore, not smoking is a way to reduce your risk of dementia.
4. Limit your alcohol consumption
Alcohol has a complex relationship with dementia. Heavy drinking has been established as a risk factor for dementia and directly causes alcohol-related dementia.
However, there is also evidence that light to moderate alcohol intake in mid-late life could decrease your risk of dementia. Plus, red wine contains flavanols, which have been linked to a reduced risk of dementia.
DPUK Director Professor John Gallacher, also from the Department of Psychiatry, recommends limiting alcohol intake to seven units a week to account for both sides of the coin.
5. Be socially active
Another way to keep your brain active is to stay socially active. Not only does keeping in touch with friends and family have a positive effect on mood, studies have shown that it can protect against a decline in thinking skills.
Even small amounts of social interaction can make a positive difference: interacting with someone else for just 10 minutes before taking memory and attention tasks improved people's results.
6. Take part in intellectual leisure activities
To keep your brain working at its best, it's important to keep it regularly stimulated.
One way to do this is by taking part in intellectual leisure activities.
Activities identified as reducing a person's risk of dementia include reading, attending a club, manual hobbies like needlework, and arts-related activities like visiting galleries or theatres.
7. Wear hearing aids if you have hearing loss
Hearing loss was named as one of the 12 risk factors for dementia in The Lancet 2020 Commission, and is being investigated as a risk factor for dementia by our experts at Oxford.
So, if you have a hearing impairment, it's a good idea to wear a hearing aid.
8. Get enough sleep
Sleep is crucial for creating long-lasting memories, and healthy adults should get seven to nine hours of sleep each night.
Learn more about Oxford’s research on the impact of sleep on brain and mental health.
Impacts of dementia


Your Beautiful Brain workshop
Your Beautiful Brain workshop
Understanding experiences of people with dementia
Researchers from the Nuffield Department of Primary Health Care Sciences are undertaking a project to understand the experiences of people with early-stage dementia and those who care for people living with dementia.
The study will run until 2024 and is co-led by Suzanne Sayuri Ii, with funding from the NIHR. The researchers are interviewing family carers, from a range of backgrounds, on their experiences of caring for a friend or relative living with dementia, as well as interviewing 30 people with early-stage dementia.
This research will be used to produce a resource on charity website Socialcaretalk.org, forming a record for people with dementia, their families and carers to find out what helped other people when they faced similar challenges. A resource will also be developed to support health and care workers, and the people who train them.

Researchers at Oxford Population Health are investigating how to improve the experiences of people with dementia across a number of studies.
They are collaborating with colleagues from Kings College London on two randomised trials (MADE and ATTILA) of interventions designed to improve the care of elderly patients with Alzheimer’s disease, and a trial of treatment for elderly patients with late-onset schizophrenia (ATLAS2).
The Hospital at Home trial, led by Professor Sasha Shepperd, examines how providing acute care at home compares with hospital admission.
‘Our study has produced valuable information to guide policy and healthcare providers. Up until now, nobody has known whether to fully invest in Hospital at Home nationwide, or to focus on hospital care.’
Representation in research
Dr Sarah Bauermeister, from the Department of Psychiatry and Dementias Platform UK, is Principal Investigator of the Your Beautiful Brain project, which received funding from Alzheimer's Research UK to support diversity and inclusivity in dementias research, and is conducted in partnership with The Black Dementia Company.
People from African and Caribbean communities are underrepresented in dementia research. 'Your Beautiful Brain' is combatting this disparity by involving African and Caribbean artists and dementia researchers working together to deliver art workshops.
The workshops invite attendees from the African and Caribbean communities to engage with artists and each other to create art and learn about brain health.
Dr Bauermeister appeared on BBC Radio Oxford's morning show to talk about Your Beautiful Brain.

The future of dementia research
Progressing dementia research
Dementias Platform UK (DPUK) is a partnership between 29 public, private and third sector organisations, with core funding from the Medical Research Council.
Based at the University of Oxford, DPUK brings together expertise from universities, charities, and pharmaceutical and technology companies to enable crucial breakthroughs in dementia research.
DPUK focuses on the human side of dementia research, aiming to bridge the gap between early-stage scientific discoveries in laboratories and successful trials of new treatments in patients, and is directed by the Department of Psychiatry’s Professor John Gallacher.
‘One of DPUK’s most important contributions to dementia research is the vast quantity of data it makes available to researchers so we can explore the varied causes of dementia and get a much more complete picture of why some people degenerate faster than others.’
DPUK has three main strands of research, including the DPUK Data Portal, the most in-depth resource globally for longitudinal data.
Longitudinal data:
Information collected in research projects known as cohort studies that follow participants over an extended period of time
The DPUK Data Portal gives researchers access to millions of health records from dozens of these cohort studies in a single, secure repository. Analysis of this data continuously offers new insights into dementia – including the earliest signs of disease.
In February 2023, DPUK secured £2.2 million funding from the Alzheimer’s Disease Data Initiative to deliver their Democratising Dementia Data project using the Data Portal, which will support them by enabling easier access to dementia-relevant data worldwide.
‘Access to high-quality data is the biggest accelerator of scientific research. This applies especially to complex conditions like dementia. We are delighted to work with ADDI to make research-ready data globally available for dementia research.’
Dr Sarah Bauermeister speaks more on DPUK’s Data Portal
DPUK’s Trials Delivery Framework is creating an engine for testing new treatments for dementia.
Dr Vanessa Raymont from the Department of Psychiatry and DPUK’s Associate Director, outlines how the Trials Delivery Framework aims to match public volunteers with the most appropriate new dementia research studies in a Q+A.
The Experimental Medicine Incubator supports a range of innovative scientific studies investigating the root causes and underlying mechanisms of dementia in humans.
Professor James Rowe from the University of Cambridge on the Experimental Medicine Incubator
DPUK’s Great Minds register is a register for healthy study volunteers who can help contribute to dementia research by completing questionnaires and assessments that improve researchers' understanding of changing brain health.
Dr Ivan Koychev from the Department of Psychiatry describes the importance of studying dementia in its early stages and the key role data from healthy volunteers plays, in an article for The Conversation.
He describes the four key developments over the past decade that could make treatment of pre-clinical dementia possible: the ever-improving understanding of risk factors, rapid development of digital technologies, biomarker blood tests and rapid access to data through projects such as the DPUK Data Portal.




Listen to more podcasts on the future of dementia research at Oxford
Podcast series: Understanding Alzheimer's and Dementia: Oxford ARUK Public Open Day
Short talks on Alzheimer's, Dementia, current treatments and latest research, recorded at the Academic Centre, JR Hospital, Oxford
Meeting the challenges of dementia research
There are many opportunities for medical students and doctors to undertake research relevant to old age psychiatry, particularly dementia.
Dementia, future treatments and research
Professor Klaus Ebmeier is the Foundation Chair of Old Age Psychiatry. In this interview he gives his point of view on dementia, normal aging and why new treatments are not yet effective.
MRC Dementias platform
Professor Clare Mackay, Department of Psychiatry, gives a talk for the Oxford Conference on Psychiatry and Ageing.
Are exhausts causing dementia?
The Big Questions with Oxford Sparks podcast examines the harmful effects of breathing in exhaust fumes on our bodies and brains.